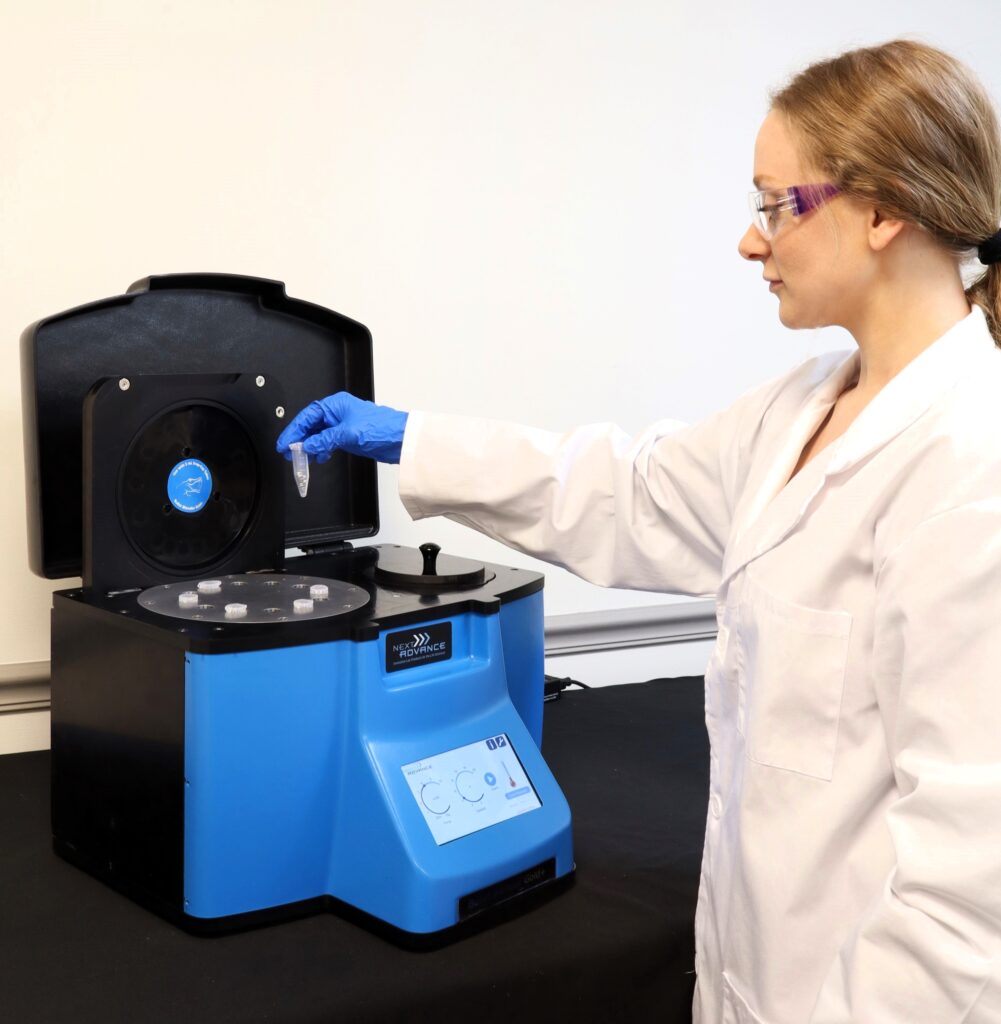
Ideal for Brain Tissue Homogenization
Do you spend lots of time and effort homogenizing brain tissue samples? The Bullet Blender® tissue homogenizer delivers high quality and superior yields. No other homogenizer comes close to delivering the Bullet Blender’s winning combination of top-quality performance and budget-friendly affordability. See below for a brain tissue homogenization protocol.
Save Time, Effort and Get Superior Results with
The Bullet Blender Homogenizer
Consistent and High Yield Results
Run up to 24 samples at the same time under microprocessor-controlled conditions, ensuring experimental reproducibility and high yield. Process samples from 10mg or less up to 3.5g.No Cross Contamination
No part of the Bullet Blender ever touches the tissue – the sample tubes are kept closed during homogenization. There are no probes to clean between samples.Samples Stay Cool
The Bullet Blenders’ innovative and elegant design provides convective cooling of the samples, so they do not heat up more than several degrees. In fact, our Gold+ models hold the sample temperature to about 4ºC.Easy and Convenient to Use
Just place beads and buffer along with your tissue sample in standard tubes, load tubes directly in the Bullet Blender, select time and speed, and press start.Risk Free Purchase
Thousands of peer-reviewed journal articles attest to the consistency and quality of the Bullet Blender homogenizer. We offer a 2 year warranty, extendable to 4 years, because our Bullet Blenders are reliable and last for many years.Brain Tissue Homogenization Protocol
Sample size |
See the Protocol |
| microcentrifuge tube model (up to 300 mg) | Small brain samples |
| 5mL tube model (100mg - 1g) | Medium brain samples |
| 50mL tube model (100mg - 3.5g) | Large brain samples |
What Else Can You Homogenize? Tough or Soft, No Problem!
The Bullet Blender can process a wide range of samples including organ tissue, cell culture, plant tissue, and small organisms. You can homogenize samples as tough as mouse femur or for gentle applications such as tissue dissociation or organelle isolation.


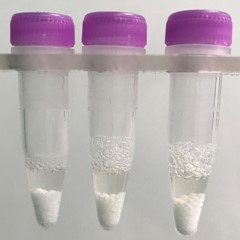
Brain tissue pieces (on beads in upper photo) are completely homogenized into the buffer (slightly darker in lower photo).
Want more guidance? Need a quote? Contact us:
Bullet Blender Models
Select Publications using the Bullet Blender to Homogenize Brain Tissue
2474232
brain
1
apa
50
date
desc
3096
https://www.nextadvance.com/wp-content/plugins/zotpress/
%7B%22status%22%3A%22success%22%2C%22updateneeded%22%3Afalse%2C%22instance%22%3Afalse%2C%22meta%22%3A%7B%22request_last%22%3A100%2C%22request_next%22%3A50%2C%22used_cache%22%3Atrue%7D%2C%22data%22%3A%5B%7B%22key%22%3A%22RHF6M76X%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Mahinrad%20et%20al.%22%2C%22parsedDate%22%3A%222018-11-26%22%2C%22numChildren%22%3A1%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3EMahinrad%2C%20S.%2C%20Bulk%2C%20M.%2C%20van%20der%20Velpen%2C%20I.%2C%20Mahfouz%2C%20A.%2C%20van%20Roon-Mom%2C%20W.%2C%20Fedarko%2C%20N.%2C%20Yasar%2C%20S.%2C%20Sabayan%2C%20B.%2C%20van%20Heemst%2C%20D.%2C%20%26amp%3B%20van%20der%20Weerd%2C%20L.%20%282018%29.%20Natriuretic%20Peptides%20in%20Post-mortem%20Brain%20Tissue%20and%20Cerebrospinal%20Fluid%20of%20Non-demented%20Humans%20and%20Alzheimer%26%23x2019%3Bs%20Disease%20Patients.%20%3Ci%3EFrontiers%20in%20Neuroscience%3C%5C%2Fi%3E%2C%20%3Ci%3E12%3C%5C%2Fi%3E%2C%20864.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.3389%5C%2Ffnins.2018.00864%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.3389%5C%2Ffnins.2018.00864%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Natriuretic%20Peptides%20in%20Post-mortem%20Brain%20Tissue%20and%20Cerebrospinal%20Fluid%20of%20Non-demented%20Humans%20and%20Alzheimer%5Cu2019s%20Disease%20Patients%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Simin%22%2C%22lastName%22%3A%22Mahinrad%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Marjolein%22%2C%22lastName%22%3A%22Bulk%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Isabelle%22%2C%22lastName%22%3A%22van%20der%20Velpen%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Ahmed%22%2C%22lastName%22%3A%22Mahfouz%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Willeke%22%2C%22lastName%22%3A%22van%20Roon-Mom%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Neal%22%2C%22lastName%22%3A%22Fedarko%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Sevil%22%2C%22lastName%22%3A%22Yasar%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Behnam%22%2C%22lastName%22%3A%22Sabayan%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Diana%22%2C%22lastName%22%3A%22van%20Heemst%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Louise%22%2C%22lastName%22%3A%22van%20der%20Weerd%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222018-11-26%22%2C%22language%22%3A%22%22%2C%22DOI%22%3A%2210.3389%5C%2Ffnins.2018.00864%22%2C%22ISSN%22%3A%221662-453X%22%2C%22url%22%3A%22https%3A%5C%2F%5C%2Fwww.frontiersin.org%5C%2Farticle%5C%2F10.3389%5C%2Ffnins.2018.00864%5C%2Ffull%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222020-01-24T18%3A02%3A26Z%22%7D%7D%2C%7B%22key%22%3A%2229NFINZ9%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Kim%20et%20al.%22%2C%22parsedDate%22%3A%222016-10-01%22%2C%22numChildren%22%3A2%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3EKim%2C%20J.%20M.%2C%20Park%2C%20S.%20K.%2C%20Guo%2C%20T.%20J.%2C%20Kang%2C%20J.%20Y.%2C%20Ha%2C%20J.%20S.%2C%20Lee%2C%20D.%20S.%2C%20Lee%2C%20U.%2C%20%26amp%3B%20Heo%2C%20H.%20J.%20%282016%29.%20Anti-amnesic%20effect%20of%20Dendropanax%20morbifera%20via%20JNK%20signaling%20pathway%20on%20cognitive%20dysfunction%20in%20high-fat%20diet-induced%20diabetic%20mice.%20%3Ci%3EBehavioural%20Brain%20Research%3C%5C%2Fi%3E%2C%20%3Ci%3E312%3C%5C%2Fi%3E%2C%2039%26%23x2013%3B54.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2Fj.bbr.2016.06.013%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2Fj.bbr.2016.06.013%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Anti-amnesic%20effect%20of%20Dendropanax%20morbifera%20via%20JNK%20signaling%20pathway%20on%20cognitive%20dysfunction%20in%20high-fat%20diet-induced%20diabetic%20mice%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Jong%20Min%22%2C%22lastName%22%3A%22Kim%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Seon%20Kyeong%22%2C%22lastName%22%3A%22Park%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Tian%20Jiao%22%2C%22lastName%22%3A%22Guo%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Jin%20Yong%22%2C%22lastName%22%3A%22Kang%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Jeong%20Su%22%2C%22lastName%22%3A%22Ha%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Du%20Sang%22%2C%22lastName%22%3A%22Lee%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Uk%22%2C%22lastName%22%3A%22Lee%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Ho%20Jin%22%2C%22lastName%22%3A%22Heo%22%7D%5D%2C%22abstractNote%22%3A%22The%20ameliorating%20effects%20of%20the%20ethyl%20acetate%20fraction%20from%20Dendropanax%20morbifera%20%28EFDM%29%20on%20cognitive%20impairment%20in%20high-fat%20diet%20%28HFD%29-induced%20diabetic%20mice%20were%20examined%20by%20measuring%20its%20possible%20pharmacological%20activities.%20Administration%20of%20EFDM%20%2820%20and%2050%20mg%5C%2Fkg%20body%20weight%29%20in%20HFD-induced%20diabetic%20mice%20significantly%20improved%20glucose%20tolerance%20status%20in%20the%20intraperitoneal%20glucose%20tolerance%20test%20%28IPGTT%29.%20In%20animal%20experiments%20using%20Y-maze%2C%20passive%20avoidance%20and%20Morris%20water%20maze%20tests%2C%20the%20cognitive%20and%20behavioral%20disorders%20in%20HFD-induced%20diabetic%20mice%20were%20considerably%20recovered%20by%20regulating%20cholinergic%20systems%2C%20including%20acetylcholine%20%28ACh%29%20levels%20and%20acetylcholinesterase%20%28AChE%29%20inhibition%2C%20and%20antioxidant%20systems%2C%20including%20superoxide%20dismutase%20%28SOD%29%2C%20glutathione%20%28GSH%29%2C%20oxidized%20GSH%2C%20and%20malondialdehyde%20%28MDA%29%20levels.%20Furthermore%2C%20HFD-induced%20abnormal%20activity%20of%20mitochondria%20were%20also%20significantly%20protected%20by%20the%20improvement%20of%20the%20c-Jun%20N-terminal%20protein%20kinase%20%28JNK%29%20signaling%20pathway%20with%20phosphorylated%20JNK%20%28p-JNK%29%2C%20phosphorylated%20insulin%20receptor%20substrate%20%28p-IRS%29%2C%20serine%5C%2Fthreonine%20protein%20kinase%20%28Akt%29%2C%20phosphorylated%20Akt%20%28p-Akt%29%2C%20and%20phosphorylated%20tau%20%28p-tau%29.%20Finally%2C%20rutin%2C%20orientin%2C%20isoorientin%2C%20and%20luteolin-7-O-rutinoside%20as%20the%20main%20phenolics%20of%20EFDM%20were%20identified%20using%20ultra-performance%20liquid%20chromatography%5C%2Fquadrupole%20time%20of%20flight%20tandem%20mass%20spectrometry%20%28UPLC-QTOF%5C%2FMS2%29.%20These%20findings%20suggest%20that%20EFDM%20may%20have%20an%20effect%20as%20a%20multiple%20preventive%20substances%20to%20reduce%20diabetes-associated%20cognitive%20dysfunction.%22%2C%22date%22%3A%22October%201%2C%202016%22%2C%22language%22%3A%22%22%2C%22DOI%22%3A%2210.1016%5C%2Fj.bbr.2016.06.013%22%2C%22ISSN%22%3A%220166-4328%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fwww.sciencedirect.com%5C%2Fscience%5C%2Farticle%5C%2Fpii%5C%2FS0166432816303679%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222016-06-24T15%3A27%3A17Z%22%7D%7D%2C%7B%22key%22%3A%22STGJVN88%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Murray%20et%20al.%22%2C%22parsedDate%22%3A%222016-08-25%22%2C%22numChildren%22%3A2%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3EMurray%2C%20H.%20C.%2C%20Low%2C%20V.%20F.%2C%20Swanson%2C%20M.%20E.%20V.%2C%20Dieriks%2C%20B.%20V.%2C%20Turner%2C%20C.%2C%20Faull%2C%20R.%20L.%20M.%2C%20%26amp%3B%20Curtis%2C%20M.%20A.%20%282016%29.%20Distribution%20of%20PSA-NCAM%20in%20normal%2C%20Alzheimer%26%23x2019%3Bs%20and%20Parkinson%26%23x2019%3Bs%20disease%20human%20brain.%20%3Ci%3ENeuroscience%3C%5C%2Fi%3E%2C%20%3Ci%3E330%3C%5C%2Fi%3E%2C%20359%26%23x2013%3B375.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2Fj.neuroscience.2016.06.003%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2Fj.neuroscience.2016.06.003%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Distribution%20of%20PSA-NCAM%20in%20normal%2C%20Alzheimer%5Cu2019s%20and%20Parkinson%5Cu2019s%20disease%20human%20brain%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Helen%20C.%22%2C%22lastName%22%3A%22Murray%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Victoria%20F.%22%2C%22lastName%22%3A%22Low%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Molly%20E.%20V.%22%2C%22lastName%22%3A%22Swanson%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Birger%20V.%22%2C%22lastName%22%3A%22Dieriks%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Clinton%22%2C%22lastName%22%3A%22Turner%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Richard%20L.%20M.%22%2C%22lastName%22%3A%22Faull%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Maurice%20A.%22%2C%22lastName%22%3A%22Curtis%22%7D%5D%2C%22abstractNote%22%3A%22Polysialated%20neural%20cell%20adhesion%20molecule%20%28PSA-NCAM%29%20is%20a%20membrane%20bound%20glycoprotein%20widely%20expressed%20during%20nervous%20system%20development.%20While%20commonly%20described%20in%20the%20neurogenic%20niches%20of%20the%20adult%20human%20brain%2C%20there%20is%20limited%20evidence%20of%20its%20distribution%20in%20other%20brain%20regions.%20PSA-NCAM%20is%20an%20important%20regulator%20of%20cell%5Cu2013cell%20interactions%20and%20facilitates%20cell%20migration%20and%20plasticity.%20Recent%20evidence%20suggests%20these%20functions%20may%20be%20altered%20in%20neurodegenerative%20diseases%20such%20as%20Alzheimer%5Cu2019s%20%28AD%29%20and%20Parkinson%5Cu2019s%20disease%20%28PD%29.%20This%20study%20provides%20a%20detailed%20description%20of%20the%20PSA-NCAM%20distribution%20throughout%20the%20human%20brain%20and%20quantitatively%20compares%20the%20staining%20load%20in%20cortical%20regions%20and%20sub-cortical%20structures%20between%20the%20control%2C%20AD%20and%20PD%20brain.%20Our%20results%20provide%20evidence%20of%20widespread%2C%20yet%20specific%2C%20PSA-NCAM%20expression%20throughout%20the%20human%20brain%20including%20regions%20devoid%20of%20PSA-NCAM%20in%20the%20rodent%20brain%20such%20as%20the%20caudate%20nucleus%20%28CN%29%20and%20cerebellum%20%28CB%29.%20We%20also%20detected%20a%20significant%20reduction%20in%20PSA-NCAM%20load%20in%20the%20entorhinal%20cortex%20%28EC%29%20of%20cases%20that%20was%20inversely%20correlated%20with%20hyperphosphorylated%20tau%20load.%20These%20results%20demonstrate%20that%20PSA-NCAM-mediated%20structural%20plasticity%20may%20not%20be%20limited%20to%20neurogenic%20niches%20and%20is%20conserved%20in%20the%20aged%20brain.%20We%20also%20provide%20evidence%20that%20PSA-NCAM%20is%20reduced%20in%20the%20EC%2C%20a%20region%20severely%20affected%20by%20AD%20pathology.%22%2C%22date%22%3A%22August%2025%2C%202016%22%2C%22language%22%3A%22%22%2C%22DOI%22%3A%2210.1016%5C%2Fj.neuroscience.2016.06.003%22%2C%22ISSN%22%3A%220306-4522%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fwww.sciencedirect.com%5C%2Fscience%5C%2Farticle%5C%2Fpii%5C%2FS0306452216302330%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222016-06-24T16%3A26%3A54Z%22%7D%7D%2C%7B%22key%22%3A%22JMHTTBSF%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22David%20et%20al.%22%2C%22parsedDate%22%3A%222016-06-09%22%2C%22numChildren%22%3A2%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3EDavid%2C%20C.%20N.%2C%20Frias%2C%20E.%20S.%2C%20Szu%2C%20J.%20I.%2C%20Vieira%2C%20P.%20A.%2C%20Hubbard%2C%20J.%20A.%2C%20Lovelace%2C%20J.%2C%20Michael%2C%20M.%2C%20Worth%2C%20D.%2C%20McGovern%2C%20K.%20E.%2C%20Ethell%2C%20I.%20M.%2C%20Stanley%2C%20B.%20G.%2C%20Korzus%2C%20E.%2C%20Fiacco%2C%20T.%20A.%2C%20Binder%2C%20D.%20K.%2C%20%26amp%3B%20Wilson%2C%20E.%20H.%20%282016%29.%20GLT-1-Dependent%20Disruption%20of%20CNS%20Glutamate%20Homeostasis%20and%20Neuronal%20Function%20by%20the%20Protozoan%20Parasite%20Toxoplasma%20gondii.%20%3Ci%3EPLOS%20Pathog%3C%5C%2Fi%3E%2C%20%3Ci%3E12%3C%5C%2Fi%3E%286%29%2C%20e1005643.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1371%5C%2Fjournal.ppat.1005643%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1371%5C%2Fjournal.ppat.1005643%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22GLT-1-Dependent%20Disruption%20of%20CNS%20Glutamate%20Homeostasis%20and%20Neuronal%20Function%20by%20the%20Protozoan%20Parasite%20Toxoplasma%20gondii%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Cl%5Cu00e9ment%20N.%22%2C%22lastName%22%3A%22David%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Elma%20S.%22%2C%22lastName%22%3A%22Frias%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Jenny%20I.%22%2C%22lastName%22%3A%22Szu%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Philip%20A.%22%2C%22lastName%22%3A%22Vieira%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Jacqueline%20A.%22%2C%22lastName%22%3A%22Hubbard%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Jonathan%22%2C%22lastName%22%3A%22Lovelace%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Marena%22%2C%22lastName%22%3A%22Michael%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Danielle%22%2C%22lastName%22%3A%22Worth%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Kathryn%20E.%22%2C%22lastName%22%3A%22McGovern%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Iryna%20M.%22%2C%22lastName%22%3A%22Ethell%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22B.%20Glenn%22%2C%22lastName%22%3A%22Stanley%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Edward%22%2C%22lastName%22%3A%22Korzus%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Todd%20A.%22%2C%22lastName%22%3A%22Fiacco%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Devin%20K.%22%2C%22lastName%22%3A%22Binder%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Emma%20H.%22%2C%22lastName%22%3A%22Wilson%22%7D%5D%2C%22abstractNote%22%3A%22Author%20Summary%20%20%20The%20protozoan%20parasite%20%20Toxoplasma%20gondii%20%20infects%20a%20third%20of%20the%20world%5Cu2019s%20population%20and%20causes%20a%20chronic%20lifelong%20infection%20in%20the%20brain%20of%20the%20host.%20The%20consequences%20of%20such%20an%20infection%20are%20poorly%20understood.%20Here%2C%20we%20demonstrate%20that%20%20Toxoplasma%20%20infection%20can%20induce%20profound%20changes%20in%20astrocyte%20physiology%20leading%20to%20significant%20disruption%20of%20neuronal%20networks.%20Pathology%20can%20be%20rescued%20by%20upregulating%20the%20astrocytic%20glutamate%20transporter%2C%20GLT-1%2C%20restoring%20concentrations%20of%20extracellular%20glutamate%20and%20EEG%20power.%20We%20suggest%20that%20such%20global%20dysregulation%20of%20neurotransmitters%20should%20be%20considered%20when%20determining%20the%20effects%20of%20infection%20on%20the%20CNS.%22%2C%22date%22%3A%22Jun%209%2C%202016%22%2C%22language%22%3A%22%22%2C%22DOI%22%3A%2210.1371%5C%2Fjournal.ppat.1005643%22%2C%22ISSN%22%3A%221553-7374%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fjournals.plos.org%5C%2Fplospathogens%5C%2Farticle%3Fid%3D10.1371%5C%2Fjournal.ppat.1005643%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222016-06-24T16%3A54%3A14Z%22%7D%7D%2C%7B%22key%22%3A%227N3HD2CU%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Perland%20et%20al.%22%2C%22parsedDate%22%3A%222016-06-07%22%2C%22numChildren%22%3A2%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3EPerland%2C%20E.%2C%20Lekholm%2C%20E.%2C%20Eriksson%2C%20M.%20M.%2C%20Bagchi%2C%20S.%2C%20Arapi%2C%20V.%2C%20%26amp%3B%20Fredriksson%2C%20R.%20%282016%29.%20The%20Putative%20SLC%20Transporters%20Mfsd5%20and%20Mfsd11%20Are%20Abundantly%20Expressed%20in%20the%20Mouse%20Brain%20and%20Have%20a%20Potential%20Role%20in%20Energy%20Homeostasis.%20%3Ci%3EPLOS%20ONE%3C%5C%2Fi%3E%2C%20%3Ci%3E11%3C%5C%2Fi%3E%286%29%2C%20e0156912.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1371%5C%2Fjournal.pone.0156912%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1371%5C%2Fjournal.pone.0156912%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22The%20Putative%20SLC%20Transporters%20Mfsd5%20and%20Mfsd11%20Are%20Abundantly%20Expressed%20in%20the%20Mouse%20Brain%20and%20Have%20a%20Potential%20Role%20in%20Energy%20Homeostasis%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Emelie%22%2C%22lastName%22%3A%22Perland%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Emilia%22%2C%22lastName%22%3A%22Lekholm%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Mikaela%20M.%22%2C%22lastName%22%3A%22Eriksson%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Sonchita%22%2C%22lastName%22%3A%22Bagchi%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Vasiliki%22%2C%22lastName%22%3A%22Arapi%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Robert%22%2C%22lastName%22%3A%22Fredriksson%22%7D%5D%2C%22abstractNote%22%3A%22Background%20%20%20Solute%20carriers%20%28SLCs%29%20are%20membrane%20bound%20transporters%20responsible%20for%20the%20movement%20of%20soluble%20molecules%20such%20as%20amino%20acids%2C%20ions%2C%20nucleotides%2C%20neurotransmitters%20and%20oligopeptides%20over%20cellular%20membranes.%20At%20present%2C%20there%20are%20395%20SLCs%20identified%20in%20humans%2C%20where%20about%2040%25%20are%20still%20uncharacterized%20with%20unknown%20expression%20and%5C%2For%20function%28s%29.%20Here%20we%20have%20studied%20two%20uncharacterized%20atypical%20SLCs%20that%20belong%20to%20the%20Major%20Facilitator%20Superfamily%20Pfam%20clan%2C%20Major%20facilitator%20superfamily%20domain%205%20%28MFSD5%29%20and%20Major%20facilitator%20superfamily%20domain%2011%20%28MFSD11%29.%20We%20provide%20fundamental%20information%20about%20the%20histology%20in%20mice%20as%20well%20as%20data%20supporting%20their%20disposition%20to%20regulate%20expression%20levels%20to%20keep%20the%20energy%20homeostasis.%20%20%20%20%20%20%20Results%20%20%20In%20mice%20subjected%20to%20starvation%20or%20high-fat%20diet%2C%20the%20mRNA%20expression%20of%20%20Mfsd5%20%20was%20significantly%20down-regulated%20%28P%26lt%3B0.001%29%20in%20food%20regulatory%20brain%20areas%20whereas%20%20Mfsd11%20%20was%20significantly%20up-regulated%20in%20mice%20subjected%20to%20either%20starvation%20%28P%26lt%3B0.01%29%20or%20high-fat%20diet%20%28P%26lt%3B0.001%29.%20qRT-PCR%20analysis%20on%20wild%20type%20tissues%20demonstrated%20that%20both%20%20Mfsd5%20%20and%20%20Mfsd11%20%20have%20a%20wide%20central%20and%20peripheral%20mRNA%20distribution%2C%20and%20immunohistochemistry%20was%20utilized%20to%20display%20the%20abundant%20protein%20expression%20in%20the%20mouse%20embryo%20and%20the%20adult%20mouse%20brain.%20Both%20proteins%20are%20expressed%20in%20excitatory%20and%20inhibitory%20neurons%2C%20but%20not%20in%20astrocytes.%20%20%20%20%20%20%20Conclusions%20%20%20%20Mfsd5%20%20and%20%20Mfsd11%20%20are%20both%20affected%20by%20altered%20energy%20homeostasis%2C%20suggesting%20plausible%20involvement%20in%20the%20energy%20regulation.%20Moreover%2C%20the%20first%20histological%20mapping%20of%20MFSD5%20and%20MFSD11%20shows%20ubiquitous%20expression%20in%20the%20periphery%20and%20the%20central%20nervous%20system%20of%20mice%2C%20where%20the%20proteins%20are%20expressed%20in%20excitatory%20and%20inhibitory%20mouse%20brain%20neurons.%22%2C%22date%22%3A%22Jun%207%2C%202016%22%2C%22language%22%3A%22%22%2C%22DOI%22%3A%2210.1371%5C%2Fjournal.pone.0156912%22%2C%22ISSN%22%3A%221932-6203%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fjournals.plos.org%5C%2Fplosone%5C%2Farticle%3Fid%3D10.1371%5C%2Fjournal.pone.0156912%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222016-06-10T19%3A32%3A40Z%22%7D%7D%2C%7B%22key%22%3A%2273UCHNEK%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Kumar%20et%20al.%22%2C%22parsedDate%22%3A%222016-05-23%22%2C%22numChildren%22%3A2%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3EKumar%2C%20M.%2C%20Belcaid%2C%20M.%2C%20%26amp%3B%20Nerurkar%2C%20V.%20R.%20%282016%29.%20Identification%20of%20host%20genes%20leading%20to%20West%20Nile%20virus%20encephalitis%20in%20mice%20brain%20using%20RNA-seq%20analysis.%20%3Ci%3EScientific%20Reports%3C%5C%2Fi%3E%2C%20%3Ci%3E6%3C%5C%2Fi%3E.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1038%5C%2Fsrep26350%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1038%5C%2Fsrep26350%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Identification%20of%20host%20genes%20leading%20to%20West%20Nile%20virus%20encephalitis%20in%20mice%20brain%20using%20RNA-seq%20analysis%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Mukesh%22%2C%22lastName%22%3A%22Kumar%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Mahdi%22%2C%22lastName%22%3A%22Belcaid%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Vivek%20R.%22%2C%22lastName%22%3A%22Nerurkar%22%7D%5D%2C%22abstractNote%22%3A%22Differential%20host%20responses%20may%20be%20critical%20determinants%20of%20distinct%20pathologies%20of%20West%20Nile%20virus%20%28WNV%29%20NY99%20%28pathogenic%29%20and%20WNV%20Eg101%20%28non-pathogenic%29%20strains.%20We%20employed%20RNA-seq%20technology%20to%20analyze%20global%20differential%20gene%20expression%20in%20WNV-infected%20mice%20brain%20and%20to%20identify%20the%20host%20cellular%20factors%20leading%20to%20lethal%20encephalitis.%20We%20identified%201%2C400%20and%20278%20transcripts%2C%20which%20were%20differentially%20expressed%20after%20WNV%20NY99%20and%20WNV%20Eg101%20infections%2C%20respectively%2C%20and%20147%20genes%20were%20common%20to%20infection%20with%20both%20the%20viruses.%20Genes%20that%20were%20up-regulated%20in%20infection%20with%20both%20the%20viruses%20were%20mainly%20associated%20with%20interferon%20signaling.%20Genes%20associated%20with%20inflammation%20and%20cell%20death%5C%2Fapoptosis%20were%20only%20expressed%20after%20WNV%20NY99%20infection.%20We%20demonstrate%20that%20differences%20in%20the%20activation%20of%20key%20pattern%20recognition%20receptors%20resulted%20in%20the%20induction%20of%20unique%20innate%20immune%20profiles%2C%20which%20corresponded%20with%20the%20induction%20of%20interferon%20and%20inflammatory%20responses.%20Pathway%20analysis%20of%20differentially%20expressed%20genes%20indicated%20that%20after%20WNV%20NY99%20infection%2C%20TREM-1%20mediated%20activation%20of%20toll-like%20receptors%20leads%20to%20the%20high%20inflammatory%20response.%20In%20conclusion%2C%20we%20have%20identified%20both%20common%20and%20specific%20responses%20to%20WNV%20NY99%20and%20WNV%20Eg101%20infections%20as%20well%20as%20genes%20linked%20to%20potential%20resistance%20to%20infection%20that%20may%20be%20targets%20for%20therapeutics.%22%2C%22date%22%3A%222016-05-23%22%2C%22language%22%3A%22%22%2C%22DOI%22%3A%2210.1038%5C%2Fsrep26350%22%2C%22ISSN%22%3A%222045-2322%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fwww.ncbi.nlm.nih.gov%5C%2Fpmc%5C%2Farticles%5C%2FPMC4876452%5C%2F%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222016-06-24T17%3A25%3A51Z%22%7D%7D%2C%7B%22key%22%3A%222D9KST4N%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Vadnie%20et%20al.%22%2C%22parsedDate%22%3A%222016-05-15%22%2C%22numChildren%22%3A2%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3EVadnie%2C%20C.%20A.%2C%20Ayers-Ringler%2C%20J.%2C%20Oliveros%2C%20A.%2C%20Abulseoud%2C%20O.%20A.%2C%20Choi%2C%20S.%2C%20Hitschfeld%2C%20M.%20J.%2C%20%26amp%3B%20Choi%2C%20D.-S.%20%282016%29.%20Antipsychotic-like%20effects%20of%20a%20neurotensin%20receptor%20type%201%20agonist.%20%3Ci%3EBehavioural%20Brain%20Research%3C%5C%2Fi%3E%2C%20%3Ci%3E305%3C%5C%2Fi%3E%2C%208%26%23x2013%3B17.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2Fj.bbr.2016.02.019%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2Fj.bbr.2016.02.019%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Antipsychotic-like%20effects%20of%20a%20neurotensin%20receptor%20type%201%20agonist%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Chelsea%20A.%22%2C%22lastName%22%3A%22Vadnie%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Jennifer%22%2C%22lastName%22%3A%22Ayers-Ringler%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Alfredo%22%2C%22lastName%22%3A%22Oliveros%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Osama%20A.%22%2C%22lastName%22%3A%22Abulseoud%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Sun%22%2C%22lastName%22%3A%22Choi%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Mario%20J.%22%2C%22lastName%22%3A%22Hitschfeld%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Doo-Sup%22%2C%22lastName%22%3A%22Choi%22%7D%5D%2C%22abstractNote%22%3A%22Although%20neurotensin%20%28NT%29%20analogs%20are%20known%20to%20produce%20antipsychotic-like%20effects%2C%20the%20therapeutic%20possibility%20of%20a%20brain%20penetrant%20NTS1%20agonist%20in%20treating%20psychiatric%20disorders%20has%20not%20been%20well%20studied.%20Here%2C%20we%20examined%20whether%20PD149163%2C%20a%20brain-penetrant%20NTS1-specific%20agonist%2C%20displays%20antipsychotic-like%20effects%20in%20C57BL%5C%2F6J%20mice%20by%20investigating%20the%20effect%20of%20PD149163%20on%20amphetamine-mediated%20hyperactivity%20and%20amphetamine-induced%20disruption%20of%20prepulse%20inhibition.%20In%20addition%2C%20we%20assessed%20the%20effect%20of%20PD149163%20on%20glycogen%20synthase%20kinase-3%20%28GSK-3%29%20activity%2C%20a%20downstream%20molecular%20target%20of%20antipsychotics%20and%20mood%20stabilizers%2C%20using%20phospho-specific%20antibodies.%20PD149163%20%280.1%20and%200.5%20mg%5C%2Fkg%29%20inhibited%20amphetamine-induced%20hyperactivity%20in%20mice%2C%20indicating%20that%20NTS1%20activation%20inhibits%20psychomotor%20agitation.%20PD149163%20%280.5%20mg%5C%2Fkg%29%20also%20increased%20prepulse%20inhibition%2C%20suggesting%20that%20NTS1%20activation%20reduces%20prepulse%20inhibition%20deficits%20which%20often%20co-occur%20with%20psychosis%20in%20humans.%20Interestingly%2C%20PD149163%20increased%20the%20inhibitory%20serine%20phosphorylation%20on%20both%20GSK-3%5Cu03b1%20and%20GSK-3%5Cu03b2%20in%20a%20dose-%20and%20time-dependent%20manner%20in%20the%20nucleus%20accumbens%20and%20medial%20prefrontal%20cortex%20of%20the%20mice.%20Moreover%2C%20PD149163%20inhibited%20GSK-3%20activity%20in%20the%20nucleus%20accumbens%20and%20medial%20prefrontal%20cortex%20in%20the%20presence%20of%20amphetamine.%20Thus%2C%20like%20most%20current%20antipsychotics%20and%20mood%20stabilizers%2C%20PD149163%20inhibited%20GSK-3%20activity%20in%20cortico-striatal%20circuitry.%20Together%2C%20our%20findings%20indicate%20that%20PD149163%20may%20be%20a%20novel%20antipsychotic.%22%2C%22date%22%3A%22May%2015%2C%202016%22%2C%22language%22%3A%22%22%2C%22DOI%22%3A%2210.1016%5C%2Fj.bbr.2016.02.019%22%2C%22ISSN%22%3A%220166-4328%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fwww.sciencedirect.com%5C%2Fscience%5C%2Farticle%5C%2Fpii%5C%2FS0166432816300869%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222016-06-10T18%3A47%3A05Z%22%7D%7D%2C%7B%22key%22%3A%22GD9AQC8W%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Hoover%20et%20al.%22%2C%22parsedDate%22%3A%222016-05-09%22%2C%22numChildren%22%3A2%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3EHoover%2C%20C.%20E.%2C%20Davenport%2C%20K.%20A.%2C%20Henderson%2C%20D.%20M.%2C%20Pulscher%2C%20L.%20A.%2C%20Mathiason%2C%20C.%20K.%2C%20Zabel%2C%20M.%20D.%2C%20%26amp%3B%20Hoover%2C%20E.%20A.%20%282016%29.%20Detection%20and%20Quantification%20of%20CWD%20Prions%20in%20Fixed%20Paraffin%20Embedded%20Tissues%20by%20Real-Time%20Quaking-Induced%20Conversion.%20%3Ci%3EScientific%20Reports%3C%5C%2Fi%3E%2C%20%3Ci%3E6%3C%5C%2Fi%3E.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1038%5C%2Fsrep25098%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1038%5C%2Fsrep25098%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Detection%20and%20Quantification%20of%20CWD%20Prions%20in%20Fixed%20Paraffin%20Embedded%20Tissues%20by%20Real-Time%20Quaking-Induced%20Conversion%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Clare%20E.%22%2C%22lastName%22%3A%22Hoover%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Kristen%20A.%22%2C%22lastName%22%3A%22Davenport%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Davin%20M.%22%2C%22lastName%22%3A%22Henderson%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Laura%20A.%22%2C%22lastName%22%3A%22Pulscher%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Candace%20K.%22%2C%22lastName%22%3A%22Mathiason%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Mark%20D.%22%2C%22lastName%22%3A%22Zabel%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Edward%20A.%22%2C%22lastName%22%3A%22Hoover%22%7D%5D%2C%22abstractNote%22%3A%22Traditional%20diagnostic%20detection%20of%20chronic%20wasting%20disease%20%28CWD%29%20relies%20on%20immunodetection%20of%20misfolded%20CWD%20prion%20protein%20%28PrPCWD%29%20by%20western%20blotting%2C%20ELISA%2C%20or%20immunohistochemistry%20%28IHC%29.%20These%20techniques%20require%20separate%20sample%20collections%20%28frozen%20and%20fixed%29%20which%20may%20result%20in%20discrepancies%20due%20to%20variation%20in%20prion%20tissue%20distribution%20and%20assay%20sensitivities%20that%20limit%20detection%20especially%20in%20early%20and%20subclinical%20infections.%20Here%2C%20we%20harness%20the%20power%20of%20real-time%20quaking%20induced%20conversion%20%28RT-QuIC%29%20to%20amplify%2C%20detect%2C%20and%20quantify%20prion%20amyloid%20seeding%20activity%20in%20fixed%20paraffin-embedded%20%28FPE%29%20tissue%20sections.%20We%20show%20that%20FPE%20RT-QuIC%20has%20greater%20detection%20sensitivity%20than%20IHC%20in%20tissues%20with%20low%20PrPCWD%20burdens%2C%20including%20those%20that%20are%20IHC-negative.%20We%20also%20employ%20amyloid%20formation%20kinetics%20to%20yield%20a%20semi-quantitative%20estimate%20of%20prion%20concentration%20in%20a%20given%20FPE%20tissue.%20We%20report%20that%20FPE%20RT-QuIC%20has%20the%20ability%20to%20enhance%20diagnostic%20and%20investigative%20detection%20of%20disease-associated%20PrPRES%20in%20prion%2C%20and%20potentially%20other%2C%20protein%20misfolding%20disease%20states.%22%2C%22date%22%3A%222016-05-09%22%2C%22language%22%3A%22%22%2C%22DOI%22%3A%2210.1038%5C%2Fsrep25098%22%2C%22ISSN%22%3A%222045-2322%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fwww.ncbi.nlm.nih.gov%5C%2Fpmc%5C%2Farticles%5C%2FPMC4860571%5C%2F%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222016-06-24T17%3A14%3A50Z%22%7D%7D%2C%7B%22key%22%3A%2274A3XBW2%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Lui%20et%20al.%22%2C%22parsedDate%22%3A%222016-05-05%22%2C%22numChildren%22%3A2%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3ELui%2C%20H.%2C%20Zhang%2C%20J.%2C%20Makinson%2C%20S.%20R.%2C%20Cahill%2C%20M.%20K.%2C%20Kelley%2C%20K.%20W.%2C%20Huang%2C%20H.-Y.%2C%20Shang%2C%20Y.%2C%20Oldham%2C%20M.%20C.%2C%20Martens%2C%20L.%20H.%2C%20Gao%2C%20F.%2C%20Coppola%2C%20G.%2C%20Sloan%2C%20S.%20A.%2C%20Hsieh%2C%20C.%20L.%2C%20Kim%2C%20C.%20C.%2C%20Bigio%2C%20E.%20H.%2C%20Weintraub%2C%20S.%2C%20Mesulam%2C%20M.-M.%2C%20Rademakers%2C%20R.%2C%20Mackenzie%2C%20I.%20R.%2C%20%26%23x2026%3B%20Huang%2C%20E.%20J.%20%282016%29.%20Progranulin%20Deficiency%20Promotes%20Circuit-Specific%20Synaptic%20Pruning%20by%20Microglia%20via%20Complement%20Activation.%20%3Ci%3ECell%3C%5C%2Fi%3E%2C%20%3Ci%3E165%3C%5C%2Fi%3E%284%29%2C%20921%26%23x2013%3B935.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2Fj.cell.2016.04.001%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2Fj.cell.2016.04.001%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Progranulin%20Deficiency%20Promotes%20Circuit-Specific%20Synaptic%20Pruning%20by%20Microglia%20via%20Complement%20Activation%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Hansen%22%2C%22lastName%22%3A%22Lui%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Jiasheng%22%2C%22lastName%22%3A%22Zhang%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Stefanie%5Cu00a0R.%22%2C%22lastName%22%3A%22Makinson%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Michelle%5Cu00a0K.%22%2C%22lastName%22%3A%22Cahill%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Kevin%5Cu00a0W.%22%2C%22lastName%22%3A%22Kelley%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Hsin-Yi%22%2C%22lastName%22%3A%22Huang%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Yulei%22%2C%22lastName%22%3A%22Shang%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Michael%5Cu00a0C.%22%2C%22lastName%22%3A%22Oldham%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Lauren%5Cu00a0Herl%22%2C%22lastName%22%3A%22Martens%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Fuying%22%2C%22lastName%22%3A%22Gao%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Giovanni%22%2C%22lastName%22%3A%22Coppola%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Steven%5Cu00a0A.%22%2C%22lastName%22%3A%22Sloan%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Christine%5Cu00a0L.%22%2C%22lastName%22%3A%22Hsieh%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Charles%5Cu00a0C.%22%2C%22lastName%22%3A%22Kim%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Eileen%5Cu00a0H.%22%2C%22lastName%22%3A%22Bigio%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Sandra%22%2C%22lastName%22%3A%22Weintraub%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Marek-Marsel%22%2C%22lastName%22%3A%22Mesulam%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Rosa%22%2C%22lastName%22%3A%22Rademakers%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Ian%5Cu00a0R.%22%2C%22lastName%22%3A%22Mackenzie%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22William%5Cu00a0W.%22%2C%22lastName%22%3A%22Seeley%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Anna%22%2C%22lastName%22%3A%22Karydas%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Bruce%5Cu00a0L.%22%2C%22lastName%22%3A%22Miller%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Barbara%22%2C%22lastName%22%3A%22Borroni%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Roberta%22%2C%22lastName%22%3A%22Ghidoni%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Robert%5Cu00a0V.%22%2C%22lastName%22%3A%22Farese%20Jr.%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Jeanne%5Cu00a0T.%22%2C%22lastName%22%3A%22Paz%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Ben%5Cu00a0A.%22%2C%22lastName%22%3A%22Barres%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Eric%5Cu00a0J.%22%2C%22lastName%22%3A%22Huang%22%7D%5D%2C%22abstractNote%22%3A%22Summary%5CnMicroglia%20maintain%20homeostasis%20in%20the%20brain%2C%20but%20whether%20aberrant%20microglial%20activation%20can%20cause%20neurodegeneration%20remains%20controversial.%20Here%2C%20we%20use%20transcriptome%20profiling%20to%20demonstrate%20that%20deficiency%20in%20frontotemporal%20dementia%20%28FTD%29%20gene%20progranulin%20%28Grn%29%20leads%20to%20an%20age-dependent%2C%20progressive%20upregulation%20of%20lysosomal%20and%20innate%20immunity%20genes%2C%20increased%20complement%20production%2C%20and%20enhanced%20synaptic%20pruning%20in%20microglia.%20During%20aging%2C%20Grn%5Cu2212%5C%2F%5Cu2212%20mice%20show%20profound%20microglia%20infiltration%20and%20preferential%20elimination%20of%20inhibitory%20synapses%20in%20the%20ventral%20thalamus%2C%20which%20lead%20to%20hyperexcitability%20in%20the%20thalamocortical%20circuits%20and%20obsessive-compulsive%20disorder%20%28OCD%29-like%20grooming%20behaviors.%20Remarkably%2C%20deleting%20C1qa%20gene%20significantly%20reduces%20synaptic%20pruning%20by%20Grn%5Cu2212%5C%2F%5Cu2212%20microglia%20and%20mitigates%20neurodegeneration%2C%20behavioral%20phenotypes%2C%20and%20premature%20mortality%20in%20Grn%5Cu2212%5C%2F%5Cu2212%20mice.%20Together%2C%20our%20results%20uncover%20a%20previously%20unrecognized%20role%20of%20progranulin%20in%20suppressing%20aberrant%20microglia%20activation%20during%20aging.%20These%20results%20represent%20an%20important%20conceptual%20advance%20that%20complement%20activation%20and%20microglia-mediated%20synaptic%20pruning%20are%20major%20drivers%2C%20rather%20than%20consequences%2C%20of%20neurodegeneration%20caused%20by%20progranulin%20deficiency.%22%2C%22date%22%3A%22May%205%2C%202016%22%2C%22language%22%3A%22%22%2C%22DOI%22%3A%2210.1016%5C%2Fj.cell.2016.04.001%22%2C%22ISSN%22%3A%220092-8674%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fwww.sciencedirect.com%5C%2Fscience%5C%2Farticle%5C%2Fpii%5C%2FS0092867416303920%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222016-06-10T19%3A51%3A10Z%22%7D%7D%2C%7B%22key%22%3A%22QKMNGX7B%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Zeng%20et%20al.%22%2C%22parsedDate%22%3A%222016-03-16%22%2C%22numChildren%22%3A2%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3EZeng%2C%20X.%2C%20Wang%2C%20H.%2C%20Xing%2C%20X.%2C%20Wang%2C%20Q.%2C%20%26amp%3B%20Li%2C%20W.%20%282016%29.%20Dexmedetomidine%20Protects%20against%20Transient%20Global%20Cerebral%20Ischemia%5C%2FReperfusion%20Induced%20Oxidative%20Stress%20and%20Inflammation%20in%20Diabetic%20Rats.%20%3Ci%3EPLOS%20ONE%3C%5C%2Fi%3E%2C%20%3Ci%3E11%3C%5C%2Fi%3E%283%29%2C%20e0151620.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1371%5C%2Fjournal.pone.0151620%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1371%5C%2Fjournal.pone.0151620%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Dexmedetomidine%20Protects%20against%20Transient%20Global%20Cerebral%20Ischemia%5C%2FReperfusion%20Induced%20Oxidative%20Stress%20and%20Inflammation%20in%20Diabetic%20Rats%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Xianzhang%22%2C%22lastName%22%3A%22Zeng%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Honglei%22%2C%22lastName%22%3A%22Wang%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Xichun%22%2C%22lastName%22%3A%22Xing%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Qi%22%2C%22lastName%22%3A%22Wang%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Wenzhi%22%2C%22lastName%22%3A%22Li%22%7D%5D%2C%22abstractNote%22%3A%22Background%20%20%20Transient%20global%20cerebral%20ischemia%5C%2Freperfusion%20%28I%5C%2FR%29%20is%20a%20major%20perioperative%20complication%2C%20and%20diabetes%20increases%20the%20response%20of%20oxidative%20stress%20and%20inflammation%20induced%20by%20I%5C%2FR.%20The%20objective%20of%20this%20study%20was%20to%20determine%20the%20protective%20effect%20of%20dexmedetomidine%20against%20transient%20global%20cerebral%20ischemia%5C%2Freperfusion%20induced%20oxidative%20stress%20and%20inflammation%20in%20diabetic%20rats.%20%20%20%20%20%20%20Methods%20%20%20Sixty-four%20rats%20were%20assigned%20into%20four%20experimental%20groups%3A%20normoglycemia%2C%20normoglycemia%20%2B%20dexmedetomidine%2C%20hyperglycemia%2C%20and%20hyperglycemia%20%2B%20dexmedetomidine%20and%20all%20subsequent%20neurological%20examinations%20were%20evaluated%20by%20a%20blinded%20observer.%20Damage%20to%20the%20brain%20was%20histologically%20assessed%20using%20the%20TUNEL%20staining%20method%20while%20western%20blotting%20was%20used%20to%20investigate%20changes%20in%20the%20expression%20levels%20of%20apoptosis-related%20proteins%20as%20well%20as%20the%20microglia%20marker%2C%20ionized%20calcium-binding%20adapter%20molecule%201%20%28Iba1%29.%20Water%20content%20in%20the%20brain%20was%20also%20analyzed.%20In%20addition%2C%20hippocampal%20concentrations%20of%20malondialdehyde%20%28MDA%29%20and%20Nox2%20%28a%20member%20of%20the%20Nox%20family%20of%20NADPH%20oxidases%29%2C%20and%20the%20activity%20of%20superoxide%20dismutase%20and%20catalase%20were%20analyzed.%20Finally%2C%20changes%20in%20serum%20concentrations%20of%20tumor%20necrosis%20factor-%5Cu03b1%20%28TNF-%5Cu03b1%29%20and%20interleukin%20%28IL%29-6%20were%20detected.%20%20%20%20%20%20%20Results%20%20%20Results%20showed%20that%20diabetes%20increased%20brain%20water%20content%2C%20the%20number%20of%20apoptotic%20neurons%2C%20early%20neurological%20deficit%20scores%2C%20oxidative%20stress%20%28MDA%20and%20Nox2%29%20and%20inflammation%20%28pro-inflammatory%20cytokines%20including%20TNF-%5Cu03b1%20and%20IL-6%29%20levels%20following%20transient%20global%20I%5C%2FR%20injury%2C%20but%20that%20these%20symptoms%20were%20attenuated%20following%20administration%20of%20dexmedetomidine.%20%20%20%20%20%20%20Conclusions%20%20%20These%20findings%20suggest%20that%20dexmedetomidine%20can%20significantly%20alleviate%20damage%20resulting%20from%20I%5C%2FR%2C%20and%20this%20mechanism%20may%20be%20related%20to%20a%20reduction%20in%20both%20oxidative%20stress%20and%20inflammation%20which%20is%20normally%20associated%20with%20I%5C%2FR.%22%2C%22date%22%3A%22Mar%2016%2C%202016%22%2C%22language%22%3A%22%22%2C%22DOI%22%3A%2210.1371%5C%2Fjournal.pone.0151620%22%2C%22ISSN%22%3A%221932-6203%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fjournals.plos.org%5C%2Fplosone%5C%2Farticle%3Fid%3D10.1371%5C%2Fjournal.pone.0151620%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222016-06-10T19%3A47%3A20Z%22%7D%7D%2C%7B%22key%22%3A%22Q7IP8WMR%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Ayers-Ringler%20et%20al.%22%2C%22parsedDate%22%3A%222016-03-11%22%2C%22numChildren%22%3A2%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3EAyers-Ringler%2C%20J.%20R.%2C%20Oliveros%2C%20A.%2C%20Qiu%2C%20Y.%2C%20Lindberg%2C%20D.%20M.%2C%20Hinton%2C%20D.%20J.%2C%20Moore%2C%20R.%20M.%2C%20Dasari%2C%20S.%2C%20%26amp%3B%20Choi%2C%20D.-S.%20%282016%29.%20Label-Free%20Proteomic%20Analysis%20of%20Protein%20Changes%20in%20the%20Striatum%20during%20Chronic%20Ethanol%20Use%20and%20Early%20Withdrawal.%20%3Ci%3EFrontiers%20in%20Behavioral%20Neuroscience%3C%5C%2Fi%3E%2C%20%3Ci%3E10%3C%5C%2Fi%3E.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.3389%5C%2Ffnbeh.2016.00046%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.3389%5C%2Ffnbeh.2016.00046%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Label-Free%20Proteomic%20Analysis%20of%20Protein%20Changes%20in%20the%20Striatum%20during%20Chronic%20Ethanol%20Use%20and%20Early%20Withdrawal%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Jennifer%20R.%22%2C%22lastName%22%3A%22Ayers-Ringler%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Alfredo%22%2C%22lastName%22%3A%22Oliveros%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Yanyan%22%2C%22lastName%22%3A%22Qiu%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Daniel%20M.%22%2C%22lastName%22%3A%22Lindberg%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22David%20J.%22%2C%22lastName%22%3A%22Hinton%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Raymond%20M.%22%2C%22lastName%22%3A%22Moore%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Surendra%22%2C%22lastName%22%3A%22Dasari%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Doo-Sup%22%2C%22lastName%22%3A%22Choi%22%7D%5D%2C%22abstractNote%22%3A%22The%20molecular%20mechanisms%20underlying%20the%20neuronal%20signaling%20changes%20in%20alcohol%20addiction%20and%20withdrawal%20are%20complex%20and%20multifaceted.%20The%20cortico-striatal%20circuit%20is%20highly%20implicated%20in%20these%20processes%2C%20and%20the%20striatum%20plays%20a%20significant%20role%20not%20only%20in%20the%20early%20stages%20of%20addiction%2C%20but%20in%20the%20developed-addictive%20state%20as%20well%2C%20including%20withdrawal%20symptoms.%20Transcriptional%20analysis%20is%20a%20useful%20method%20for%20determining%20changes%20in%20gene%20expression%2C%20however%2C%20the%20results%20do%20not%20always%20accurately%20correlate%20with%20protein%20levels.%20In%20this%20study%2C%20we%20employ%20label-free%20proteomic%20analysis%20to%20determine%20changes%20in%20protein%20expression%20within%20the%20striatum%20during%20chronic%20ethanol%20use%20and%20early%20withdrawal.%20The%20striatum%2C%20composed%20primarily%20of%20medium%20spiny%20GABAergic%20neurons%2C%20glutamatergic%20and%20dopaminergic%20nerve%20terminals%20and%20astrocytes%2C%20is%20relatively%20homogeneous%20for%20proteomic%20analysis.%20We%20were%20able%20to%20analyze%20more%20than%205000%20proteins%20from%20both%20the%20dorsal%20%28caudate%20and%20putamen%29%20and%20ventral%20%28nucleus%20accumbens%29%20striatum%20and%20identified%20significant%20changes%20following%20chronic%20intermittent%20ethanol%20exposure%20and%20acute%20%288%20h%29%20withdrawal%20compared%20to%20ethanol%20na%5Cu00efve%20and%20ethanol%20exposure%20groups%20respectively.%20Our%20results%20showed%20significant%20changes%20in%20proteins%20involved%20in%20glutamate%20and%20opioid%20peptide%20signaling%2C%20and%20also%20uncovered%20novel%20pathways%20including%20mitochondrial%20function%20and%20lipid%5C%2Fcholesterol%20metabolism%2C%20as%20revealed%20by%20changes%20in%20electron%20transport%20chain%20proteins%20and%20RXR%20activation%20pathways.%20These%20results%20will%20be%20useful%20in%20the%20development%20of%20novel%20treatments%20for%20alcohol%20withdrawal%20and%20thereby%20aid%20in%20recovery%20from%20alcohol%20use%20disorder.%22%2C%22date%22%3A%222016-3-11%22%2C%22language%22%3A%22%22%2C%22DOI%22%3A%2210.3389%5C%2Ffnbeh.2016.00046%22%2C%22ISSN%22%3A%221662-5153%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fwww.ncbi.nlm.nih.gov%5C%2Fpmc%5C%2Farticles%5C%2FPMC4786553%5C%2F%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222016-06-10T18%3A35%3A09Z%22%7D%7D%2C%7B%22key%22%3A%22WRRP7BXI%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Bosch%20et%20al.%22%2C%22parsedDate%22%3A%222016-03%22%2C%22numChildren%22%3A2%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3EBosch%2C%20M.%2C%20Fajardo%2C%20A.%2C%20Alcal%26%23xE1%3B-Vida%2C%20R.%2C%20Fern%26%23xE1%3Bndez-Vidal%2C%20A.%2C%20Tebar%2C%20F.%2C%20Enrich%2C%20C.%2C%20Cardellach%2C%20F.%2C%20P%26%23xE9%3Brez-Navarro%2C%20E.%2C%20%26amp%3B%20Pol%2C%20A.%20%282016%29.%20Hepatic%20Primary%20and%20Secondary%20Cholesterol%20Deposition%20and%20Damage%20in%20Niemann-Pick%20Disease.%20%3Ci%3EThe%20American%20Journal%20of%20Pathology%3C%5C%2Fi%3E%2C%20%3Ci%3E186%3C%5C%2Fi%3E%283%29%2C%20517%26%23x2013%3B523.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2Fj.ajpath.2015.12.002%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2Fj.ajpath.2015.12.002%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Hepatic%20Primary%20and%20Secondary%20Cholesterol%20Deposition%20and%20Damage%20in%20Niemann-Pick%20Disease%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Marta%22%2C%22lastName%22%3A%22Bosch%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Alba%22%2C%22lastName%22%3A%22Fajardo%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Rafael%22%2C%22lastName%22%3A%22Alcal%5Cu00e1-Vida%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Andrea%22%2C%22lastName%22%3A%22Fern%5Cu00e1ndez-Vidal%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Francesc%22%2C%22lastName%22%3A%22Tebar%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Carlos%22%2C%22lastName%22%3A%22Enrich%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Francesc%22%2C%22lastName%22%3A%22Cardellach%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Esther%22%2C%22lastName%22%3A%22P%5Cu00e9rez-Navarro%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Albert%22%2C%22lastName%22%3A%22Pol%22%7D%5D%2C%22abstractNote%22%3A%22Niemann-Pick%20C%20disease%20is%20a%20neurovisceral%20disorder%20caused%20by%20mutations%20in%20the%20NPC%20gene%20that%20result%20in%20systemic%20accumulation%20of%20intracellular%20cholesterol.%20Although%20neurodegeneration%20defines%20the%20disease%27s%20severity%2C%20in%20most%20patients%20it%20is%20preceded%20by%20hepatic%20complications%20such%20as%20cholestatic%20jaundice%20or%20hepatomegaly.%20To%20analyze%20the%20contribution%20of%20the%20hepatic%20disease%20in%20Niemann-Pick%20C%20disease%20progression%20and%20to%20evaluate%20the%20degree%20of%20primary%20and%20secondary%20hepatic%20damage%2C%20we%20generated%20a%20transgenic%20mouse%20with%20liver-selective%20expression%20of%20NPC1%20from%20embryonic%20stages.%20Hepatic%20NPC1%20re-expression%20did%20not%20ameliorate%20the%20onset%20and%20progression%20of%20neurodegeneration%20of%20the%20NPC1-null%20animal.%20However%2C%20the%20mice%20showed%20reduced%20hepatomegalia%20and%20dramatic%2C%20although%20not%20complete%2C%20reduction%20of%20hepatic%20cholesterol%20and%20serum%20bile%20salts%2C%20bilirubin%2C%20and%20transaminase%20levels.%20Therefore%2C%20hepatic%20primary%20and%20secondary%20cholesterol%20deposition%20and%20damage%20occur%20simultaneously%20during%20Niemann-Pick%20C%20disease%20progression.%22%2C%22date%22%3A%22March%202016%22%2C%22language%22%3A%22%22%2C%22DOI%22%3A%2210.1016%5C%2Fj.ajpath.2015.12.002%22%2C%22ISSN%22%3A%220002-9440%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fwww.sciencedirect.com%5C%2Fscience%5C%2Farticle%5C%2Fpii%5C%2FS0002944015006938%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222016-06-10T18%3A33%3A53Z%22%7D%7D%2C%7B%22key%22%3A%22MKIG7QJQ%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Bakmiwewa%20et%20al.%22%2C%22parsedDate%22%3A%222016-02%22%2C%22numChildren%22%3A2%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3EBakmiwewa%2C%20S.%20M.%2C%20Weiser%2C%20S.%2C%20Grey%2C%20M.%2C%20Heng%2C%20B.%2C%20Guillemin%2C%20G.%20J.%2C%20Ball%2C%20H.%20J.%2C%20%26amp%3B%20Hunt%2C%20N.%20H.%20%282016%29.%20Synergistic%20induction%20of%20CXCL10%20by%20interferon-gamma%20and%20lymphotoxin-alpha%20in%20astrocytes%3A%20Possible%20role%20in%20cerebral%20malaria.%20%3Ci%3ECytokine%3C%5C%2Fi%3E%2C%20%3Ci%3E78%3C%5C%2Fi%3E%2C%2079%26%23x2013%3B86.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2Fj.cyto.2015.11.024%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2Fj.cyto.2015.11.024%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Synergistic%20induction%20of%20CXCL10%20by%20interferon-gamma%20and%20lymphotoxin-alpha%20in%20astrocytes%3A%20Possible%20role%20in%20cerebral%20malaria%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Supun%20M.%22%2C%22lastName%22%3A%22Bakmiwewa%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Silvia%22%2C%22lastName%22%3A%22Weiser%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Meredith%22%2C%22lastName%22%3A%22Grey%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Benjamin%22%2C%22lastName%22%3A%22Heng%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Gilles%20J.%22%2C%22lastName%22%3A%22Guillemin%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Helen%20J.%22%2C%22lastName%22%3A%22Ball%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Nicholas%20H.%22%2C%22lastName%22%3A%22Hunt%22%7D%5D%2C%22abstractNote%22%3A%22Cerebral%20malaria%20%28CM%29%20has%20a%20high%20mortality%20rate%20and%20incidence%20of%20neurological%20sequelae%20in%20survivors.%20Hypoxia%20and%20cytokine%20expression%20in%20the%20brain%20are%20two%20mechanisms%20thought%20to%20contribute%20to%20the%20pathogenesis%20of%20CM.%20The%20cytokines%20interferon%20%28IFN%29-%5Cu03b3%20and%20lymphotoxin%20%28LT%29-%5Cu03b1%20and%20the%20chemokine%20CXCL10%20are%20essential%20for%20the%20development%20of%20CM%20in%20a%20mouse%20model.%20Furthermore%2C%20serum%20IFN-%5Cu03b3%20protein%20levels%20are%20higher%20in%20human%20CM%20than%20in%20controls%2C%20and%20CXCL10%20is%20elevated%20in%20both%20serum%20and%20cerebrospinal%20fluid%20in%20Ghanaian%20paediatric%20CM%20cases.%20Astrocytes%20actively%20participate%20in%20CNS%20pathologies%2C%20becoming%20activated%20in%20response%20to%20various%20stimuli%20including%20cytokines.%20Astrocyte%20activation%20also%20occurs%20in%20murine%20and%20human%20CM.%20We%20here%20determined%20the%20responsiveness%20of%20mouse%20and%20human%20astrocytes%20to%20IFN-%5Cu03b3%20and%20LT-%5Cu03b1%2C%20with%20the%20aim%20of%20further%20elucidating%20the%20role%20of%20astrocytes%20in%20CM%20pathogenesis.%20Initially%20we%20confirmed%20that%20Ifn-%5Cu03b3%20and%20Cxcl10%20are%20expressed%20in%20the%20brain%20in%20murine%20CM%2C%20and%20that%20the%20increased%20Cxcl10%20expression%20is%20IFN-%5Cu03b3-dependant.%20IFN-%5Cu03b3%20induced%20CXCL10%20production%20in%20human%20and%20murine%20astrocytes%20in%20vitro.%20The%20degree%20of%20induction%20was%20increased%20synergistically%20in%20the%20presence%20of%20LT-%5Cu03b1.%20IFN-%5Cu03b3%20induced%20the%20expression%20of%20receptors%20for%20LT-%5Cu03b1%2C%20while%20LT-%5Cu03b1%20increased%20the%20expression%20of%20the%20receptor%20for%20IFN-%5Cu03b3%2C%20in%20the%20astrocytes.%20This%20cross-induction%20may%20explain%20the%20synergistic%20effect%20of%20the%20two%20cytokines%20on%20CXCL10%20production.%20Expression%20of%20these%20receptors%20also%20was%20upregulated%20in%20the%20brain%20in%20murine%20CM.%20The%20results%20suggest%20that%20astrocytes%20contribute%20to%20CM%20pathogenesis%20by%20producing%20CXCL10%20in%20response%20to%20IFN-%5Cu03b3%20and%20LT-%5Cu03b1.%22%2C%22date%22%3A%22February%202016%22%2C%22language%22%3A%22%22%2C%22DOI%22%3A%2210.1016%5C%2Fj.cyto.2015.11.024%22%2C%22ISSN%22%3A%221043-4666%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fwww.sciencedirect.com%5C%2Fscience%5C%2Farticle%5C%2Fpii%5C%2FS1043466615301113%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222016-06-24T16%3A31%3A25Z%22%7D%7D%2C%7B%22key%22%3A%22BQNWCAPH%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Viader%20et%20al.%22%2C%22parsedDate%22%3A%222016-01-18%22%2C%22numChildren%22%3A3%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3EViader%2C%20A.%2C%20Ogasawara%2C%20D.%2C%20Joslyn%2C%20C.%20M.%2C%20Sanchez-Alavez%2C%20M.%2C%20Mori%2C%20S.%2C%20Nguyen%2C%20W.%2C%20Conti%2C%20B.%2C%20%26amp%3B%20Cravatt%2C%20B.%20F.%20%282016%29.%20A%20chemical%20proteomic%20atlas%20of%20brain%20serine%20hydrolases%20identifies%20cell%20type-specific%20pathways%20regulating%20neuroinflammation.%20%3Ci%3EELife%3C%5C%2Fi%3E%2C%20%3Ci%3E5%3C%5C%2Fi%3E%2C%20e12345.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.7554%5C%2FeLife.12345%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.7554%5C%2FeLife.12345%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22A%20chemical%20proteomic%20atlas%20of%20brain%20serine%20hydrolases%20identifies%20cell%20type-specific%20pathways%20regulating%20neuroinflammation%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Andreu%22%2C%22lastName%22%3A%22Viader%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Daisuke%22%2C%22lastName%22%3A%22Ogasawara%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Christopher%20M.%22%2C%22lastName%22%3A%22Joslyn%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Manuel%22%2C%22lastName%22%3A%22Sanchez-Alavez%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Simone%22%2C%22lastName%22%3A%22Mori%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22William%22%2C%22lastName%22%3A%22Nguyen%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Bruno%22%2C%22lastName%22%3A%22Conti%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Benjamin%20F.%22%2C%22lastName%22%3A%22Cravatt%22%7D%5D%2C%22abstractNote%22%3A%22The%20brain%20is%20made%20up%20of%20many%20types%20of%20cells.%20These%20include%20the%20neurons%20that%20transmit%20messages%20throughout%20the%20nervous%20system%2C%20and%20microglia%2C%20which%20act%20as%20the%20first%20line%20of%20the%20brain%5Cu2019s%20immune%20defense.%20The%20activity%20of%20both%20neurons%20and%20microglia%20can%20be%20influenced%20by%20molecules%20called%20endocannabinoids%20that%20bind%20to%20proteins%20on%20the%20cells%5Cu2019%20surface.%20For%20example%2C%20endocannabinoids%20affect%20how%20a%20neuron%20responds%20to%20messages%20sent%20to%20it%20from%20a%20neighbouring%20neuron%2C%20and%20help%20microglia%20to%20regulate%20the%20inflammation%20of%20brain%20tissue.%20Enzymes%20called%20serine%20hydrolases%20play%20important%20roles%20in%20several%20different%20signaling%20processes%20in%20the%20brain%2C%20including%20those%20involving%20endocannabinoids.%20Viader%20et%20al.%20have%20now%20studied%20the%20activities%20of%20these%20enzymes%20%5Cu2013%20including%20two%20called%20DAGL%5Cu03b1%20and%20DAGL%5Cu03b2%20%5Cu2013%20in%20the%20mouse%20brain%20using%20a%20technique%20called%20activity-based%20protein%20profiling.%20This%20revealed%20that%20DAGL%5Cu03b1%20plays%20an%20important%20role%20in%20controlling%20how%20neurons%20respond%20to%20endocannabinoids%2C%20while%20DAGL%5Cu03b2%20performs%20the%20equivalent%20role%20in%20microglia.%20When%20Viader%20et%20al.%20shut%20down%20DAGL%5Cu03b2%20activity%2C%20this%20only%20affected%20endocannabinoid%20signaling%20in%20microglia.%20This%20also%20had%20the%20effect%20of%20reducing%20inflammation%20in%20the%20brain%2C%20without%20affecting%20how%20endocannabinoids%20signal%20in%20neurons.%20These%20results%20suggest%20that%20inhibitors%20of%20DAGL%5Cu03b2%20could%20offer%20a%20way%20to%20suppress%20inflammation%20in%20the%20brain%2C%20which%20may%20contribute%20to%20neuropsychiatric%20and%20neurodegenerative%20diseases%2C%20while%20preserving%20the%20normal%20pathways%20that%20neurons%20use%20to%20communicate%20with%20one%20another.%22%2C%22date%22%3A%222016%5C%2F01%5C%2F18%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.7554%5C%2FeLife.12345%22%2C%22ISSN%22%3A%222050-084X%22%2C%22url%22%3A%22https%3A%5C%2F%5C%2Felifesciences.org%5C%2Fcontent%5C%2F5%5C%2Fe12345v1%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222016-06-24T16%3A47%3A14Z%22%7D%7D%2C%7B%22key%22%3A%22IVAMXMR5%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Hallgren%20and%20Viberg%22%2C%22parsedDate%22%3A%222016-01%22%2C%22numChildren%22%3A2%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3EHallgren%2C%20S.%2C%20%26amp%3B%20Viberg%2C%20H.%20%282016%29.%20Postnatal%20exposure%20to%20PFOS%2C%20but%20not%20PBDE%2099%2C%20disturb%20dopaminergic%20gene%20transcription%20in%20the%20mouse%20CNS.%20%3Ci%3EEnvironmental%20Toxicology%20and%20Pharmacology%3C%5C%2Fi%3E%2C%20%3Ci%3E41%3C%5C%2Fi%3E%2C%20121%26%23x2013%3B126.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2Fj.etap.2015.11.016%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2Fj.etap.2015.11.016%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Postnatal%20exposure%20to%20PFOS%2C%20but%20not%20PBDE%2099%2C%20disturb%20dopaminergic%20gene%20transcription%20in%20the%20mouse%20CNS%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Stefan%22%2C%22lastName%22%3A%22Hallgren%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Henrik%22%2C%22lastName%22%3A%22Viberg%22%7D%5D%2C%22abstractNote%22%3A%22The%20CNS%20of%20breast%20feeding%20infants%20and%20toddlers%20may%20be%20exposed%20to%20persistent%20organic%20pollutants%20via%20lactational%20transfer.%20Here%2C%2010%20days%20old%20mice%20were%20exposed%20to%20single%20oral%20doses%20of%20either%20PFOS%2C%20PBDE99%20or%20vehicle%20control%20and%20were%20examined%20for%20changes%20in%20dopaminergic%20gene%20transcription%20in%20CNS%20tissue%20collected%20at%2024%20h%20or%202%20months%20post%20exposure.qPCR%20analyses%20of%20brain%20tissue%20from%20mice%20euthanized%2024%20h%20post%20exposure%20revealed%20that%20PFOS%20affected%20transcription%20of%20Dopamine%20receptor-D5%20%28DRD5%29%20in%20cerebral%20cortex%20and%20Tyrosine%20hydroxylase%20%28TH%29%20in%20the%20hippocampus.%20At%202%20months%20of%20age%2C%20mice%20neonatally%20exposed%20to%20PFOS%20displayed%20decreased%20transcription%20of%20Dopamine%20receptor-D2%20%28DRD2%29%20and%20TH%20in%20hippocampus.%20No%20significant%20changes%20in%20any%20of%20the%20tested%20genes%20were%20observed%20in%20PBDE99%20exposed%20mice.%20This%20indicates%20that%20PFOS%2C%20but%20not%20PBDE99%2C%20affects%20the%20developing%20cerebral%20dopaminergic%20system%20at%20gene%20transcriptional%20level%20in%20cortex%20and%20hippocampus%2C%20which%20may%20account%20for%20some%20of%20the%20mechanistic%20effects%20behind%20the%20aetiology%20of%20neuropsychiatric%20disorders.%22%2C%22date%22%3A%22January%202016%22%2C%22language%22%3A%22%22%2C%22DOI%22%3A%2210.1016%5C%2Fj.etap.2015.11.016%22%2C%22ISSN%22%3A%221382-6689%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fwww.sciencedirect.com%5C%2Fscience%5C%2Farticle%5C%2Fpii%5C%2FS1382668915301320%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222016-06-10T18%3A30%3A35Z%22%7D%7D%2C%7B%22key%22%3A%22978CTNF8%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Luethy%20et%20al.%22%2C%22parsedDate%22%3A%222016%22%2C%22numChildren%22%3A2%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3ELuethy%2C%20L.%20N.%2C%20Erickson%2C%20A.%20K.%2C%20Jesudhasan%2C%20P.%20R.%2C%20Ikizler%2C%20M.%2C%20Dermody%2C%20T.%20S.%2C%20%26amp%3B%20Pfeiffer%2C%20J.%20K.%20%282016%29.%20Comparison%20of%20three%20neurotropic%20viruses%20reveals%20differences%20in%20viral%20dissemination%20to%20the%20central%20nervous%20system.%20%3Ci%3EVirology%3C%5C%2Fi%3E%2C%20%3Ci%3E487%3C%5C%2Fi%3E%2C%201%26%23x2013%3B10.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2Fj.virol.2015.09.019%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2Fj.virol.2015.09.019%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Comparison%20of%20three%20neurotropic%20viruses%20reveals%20differences%20in%20viral%20dissemination%20to%20the%20central%20nervous%20system%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Lauren%20N.%22%2C%22lastName%22%3A%22Luethy%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Andrea%20K.%22%2C%22lastName%22%3A%22Erickson%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Palmy%20R.%22%2C%22lastName%22%3A%22Jesudhasan%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Mine%22%2C%22lastName%22%3A%22Ikizler%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Terence%20S.%22%2C%22lastName%22%3A%22Dermody%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Julie%20K.%22%2C%22lastName%22%3A%22Pfeiffer%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%2201%5C%2F2016%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1016%5C%2Fj.virol.2015.09.019%22%2C%22ISSN%22%3A%2200426822%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Flinkinghub.elsevier.com%5C%2Fretrieve%5C%2Fpii%5C%2FS0042682215004109%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222016-06-24T16%3A47%3A52Z%22%7D%7D%2C%7B%22key%22%3A%22PQRC934P%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Kim%20et%20al.%22%2C%22parsedDate%22%3A%222016%22%2C%22numChildren%22%3A2%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3EKim%2C%20J.%2C%20Shim%2C%20J.%2C%20Lee%2C%20S.%2C%20Cho%2C%20W.-H.%2C%20Hong%2C%20E.%2C%20Lee%2C%20J.%20H.%2C%20Han%2C%20J.-S.%2C%20Lee%2C%20H.%20J.%2C%20%26amp%3B%20Lee%2C%20K.%20W.%20%282016%29.%20Rg3-enriched%20ginseng%20extract%20ameliorates%20scopolamine-induced%20learning%20deficits%20in%20mice.%20%3Ci%3EBMC%20Complementary%20and%20Alternative%20Medicine%3C%5C%2Fi%3E%2C%20%3Ci%3E16%3C%5C%2Fi%3E%2C%2066.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1186%5C%2Fs12906-016-1050-z%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1186%5C%2Fs12906-016-1050-z%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Rg3-enriched%20ginseng%20extract%20ameliorates%20scopolamine-induced%20learning%20deficits%20in%20mice%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Jiyoung%22%2C%22lastName%22%3A%22Kim%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Jaesung%22%2C%22lastName%22%3A%22Shim%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Siyoung%22%2C%22lastName%22%3A%22Lee%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Woo-Hyun%22%2C%22lastName%22%3A%22Cho%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Eunyoung%22%2C%22lastName%22%3A%22Hong%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Jin%20Hee%22%2C%22lastName%22%3A%22Lee%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Jung-Soo%22%2C%22lastName%22%3A%22Han%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Hyong%20Joo%22%2C%22lastName%22%3A%22Lee%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Ki%20Won%22%2C%22lastName%22%3A%22Lee%22%7D%5D%2C%22abstractNote%22%3A%22Ginseng%20%28Panax%20ginseng%20C.A.%20Meyer%29%20has%20been%20used%20as%20a%20traditional%20herb%20in%20the%20treatment%20of%20many%20medical%20disorders.%20Ginsenosides%2C%20which%20are%20triterpene%20derivatives%20that%20contain%20sugar%20moieties%2C%20are%20the%20main%20pharmacological%20ingredients%20in%20ginseng.%20This%20study%20was%20designed%20to%20investigate%20the%20effect%20of%20ginsenoside%20Rg3-enriched%20ginseng%20extract%20%28Rg3GE%29%20on%20scopolamine-induced%20memory%20impairment%20in%20mice.%22%2C%22date%22%3A%222016%22%2C%22language%22%3A%22%22%2C%22DOI%22%3A%2210.1186%5C%2Fs12906-016-1050-z%22%2C%22ISSN%22%3A%221472-6882%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fdx.doi.org%5C%2F10.1186%5C%2Fs12906-016-1050-z%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222016-06-10T18%3A36%3A34Z%22%7D%7D%2C%7B%22key%22%3A%22W6EWS9HC%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Gallart-Palau%20et%20al.%22%2C%22parsedDate%22%3A%222016%22%2C%22numChildren%22%3A2%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3EGallart-Palau%2C%20X.%2C%20Serra%2C%20A.%2C%20%26amp%3B%20Sze%2C%20S.%20K.%20%282016%29.%20Enrichment%20of%20extracellular%20vesicles%20from%20tissues%20of%20the%20central%20nervous%20system%20by%20PROSPR.%20%3Ci%3EMolecular%20Neurodegeneration%3C%5C%2Fi%3E%2C%20%3Ci%3E11%3C%5C%2Fi%3E%2C%2041.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1186%5C%2Fs13024-016-0108-1%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1186%5C%2Fs13024-016-0108-1%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Enrichment%20of%20extracellular%20vesicles%20from%20tissues%20of%20the%20central%20nervous%20system%20by%20PROSPR%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Xavier%22%2C%22lastName%22%3A%22Gallart-Palau%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Aida%22%2C%22lastName%22%3A%22Serra%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Siu%20Kwan%22%2C%22lastName%22%3A%22Sze%22%7D%5D%2C%22abstractNote%22%3A%22Extracellular%20vesicles%20%28EVs%29%20act%20as%20key%20mediators%20of%20intercellular%20communication%20and%20are%20secreted%20and%20taken%20up%20by%20all%20cell%20types%20in%20the%20central%20nervous%20system%20%28CNS%29.%20While%20detailed%20study%20of%20EV-based%20signaling%20is%20likely%20to%20significantly%20advance%20our%20understanding%20of%20human%20neurobiology%2C%20the%20technical%20challenges%20of%20isolating%20EVs%20from%20CNS%20tissues%20have%20limited%20their%20characterization%20using%20%5Cu2018omics%5Cu2019%20technologies.%20We%20therefore%20developed%20a%20new%20Protein%20Organic%20Solvent%20Precipitation%20%28PROSPR%29%20method%20that%20can%20efficiently%20isolate%20the%20EV%20repertoire%20from%20human%20biological%20samples.%22%2C%22date%22%3A%222016%22%2C%22language%22%3A%22%22%2C%22DOI%22%3A%2210.1186%5C%2Fs13024-016-0108-1%22%2C%22ISSN%22%3A%221750-1326%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fdx.doi.org%5C%2F10.1186%5C%2Fs13024-016-0108-1%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222016-06-10T19%3A30%3A26Z%22%7D%7D%2C%7B%22key%22%3A%22NAQVKAPZ%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Gallart-Palau%20et%20al.%22%2C%22parsedDate%22%3A%222016%22%2C%22numChildren%22%3A2%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3EGallart-Palau%2C%20X.%2C%20Lee%2C%20B.%20S.%20T.%2C%20Adav%2C%20S.%20S.%2C%20Qian%2C%20J.%2C%20Serra%2C%20A.%2C%20Park%2C%20J.%20E.%2C%20Lai%2C%20M.%20K.%20P.%2C%20Chen%2C%20C.%20P.%2C%20Kalaria%2C%20R.%20N.%2C%20%26amp%3B%20Sze%2C%20S.%20K.%20%282016%29.%20Gender%20differences%20in%20white%20matter%20pathology%20and%20mitochondrial%20dysfunction%20in%20Alzheimer%26%23x2019%3Bs%20disease%20with%20cerebrovascular%20disease.%20%3Ci%3EMolecular%20Brain%3C%5C%2Fi%3E%2C%20%3Ci%3E9%3C%5C%2Fi%3E%2C%2027.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1186%5C%2Fs13041-016-0205-7%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1186%5C%2Fs13041-016-0205-7%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Gender%20differences%20in%20white%20matter%20pathology%20and%20mitochondrial%20dysfunction%20in%20Alzheimer%5Cu2019s%20disease%20with%20cerebrovascular%20disease%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Xavier%22%2C%22lastName%22%3A%22Gallart-Palau%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Benjamin%20S.%20T.%22%2C%22lastName%22%3A%22Lee%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Sunil%20S.%22%2C%22lastName%22%3A%22Adav%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Jingru%22%2C%22lastName%22%3A%22Qian%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Aida%22%2C%22lastName%22%3A%22Serra%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Jung%20Eun%22%2C%22lastName%22%3A%22Park%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Mitchell%20K.%20P.%22%2C%22lastName%22%3A%22Lai%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Christopher%20P.%22%2C%22lastName%22%3A%22Chen%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Raj%20N.%22%2C%22lastName%22%3A%22Kalaria%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Siu%20Kwan%22%2C%22lastName%22%3A%22Sze%22%7D%5D%2C%22abstractNote%22%3A%22Dementia%20risk%20in%20women%20is%20higher%20than%20in%20men%2C%20but%20the%20molecular%20neuropathology%20of%20this%20gender%20difference%20remains%20poorly%20defined.%20In%20this%20study%2C%20we%20used%20unbiased%2C%20discovery-driven%20quantitative%20proteomics%20to%20assess%20the%20molecular%20basis%20of%20gender%20influences%20on%20risk%20of%20Alzheimer%5Cu2019s%20disease%20with%20cerebrovascular%20disease%20%28AD%5Cu2009%2B%5Cu2009CVD%29.%22%2C%22date%22%3A%222016%22%2C%22language%22%3A%22%22%2C%22DOI%22%3A%2210.1186%5C%2Fs13041-016-0205-7%22%2C%22ISSN%22%3A%221756-6606%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fdx.doi.org%5C%2F10.1186%5C%2Fs13041-016-0205-7%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222016-06-10T19%3A40%3A07Z%22%7D%7D%2C%7B%22key%22%3A%227Q2RPX6A%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Trist%5Cu00e1n-Noguero%20et%20al.%22%2C%22parsedDate%22%3A%222015-12-21%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3ETrist%26%23xE1%3Bn-Noguero%2C%20A.%2C%20D%26%23xED%3Bez%2C%20H.%2C%20Jou%2C%20C.%2C%20Pineda%2C%20M.%2C%20Ormaz%26%23xE1%3Bbal%2C%20A.%2C%20S%26%23xE1%3Bnchez%2C%20A.%2C%20Artuch%2C%20R.%2C%20%26amp%3B%20Garcia-Cazorla%2C%20%26%23xC0%3B.%20%282015%29.%20Study%20of%20a%20fetal%20brain%20affected%20by%20a%20severe%20form%20of%20tyrosine%20hydroxylase%20deficiency%2C%20a%20rare%20cause%20of%20early%20parkinsonism.%20%3Ci%3EMetabolic%20Brain%20Disease%3C%5C%2Fi%3E.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1007%5C%2Fs11011-015-9780-z%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1007%5C%2Fs11011-015-9780-z%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Study%20of%20a%20fetal%20brain%20affected%20by%20a%20severe%20form%20of%20tyrosine%20hydroxylase%20deficiency%2C%20a%20rare%20cause%20of%20early%20parkinsonism%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Alba%22%2C%22lastName%22%3A%22Trist%5Cu00e1n-Noguero%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22H%5Cu00e9ctor%22%2C%22lastName%22%3A%22D%5Cu00edez%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Cristina%22%2C%22lastName%22%3A%22Jou%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Merc%5Cu00e8%22%2C%22lastName%22%3A%22Pineda%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Aida%22%2C%22lastName%22%3A%22Ormaz%5Cu00e1bal%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Aurora%22%2C%22lastName%22%3A%22S%5Cu00e1nchez%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Rafael%22%2C%22lastName%22%3A%22Artuch%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22%5Cu00c0ngels%22%2C%22lastName%22%3A%22Garcia-Cazorla%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222015-12-21%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1007%5C%2Fs11011-015-9780-z%22%2C%22ISSN%22%3A%220885-7490%2C%201573-7365%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Flink.springer.com%5C%2F10.1007%5C%2Fs11011-015-9780-z%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222015-12-30T15%3A59%3A02Z%22%7D%7D%2C%7B%22key%22%3A%22SK8KCHX9%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Hajkova%20et%20al.%22%2C%22parsedDate%22%3A%222015-12-11%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3EHajkova%2C%20K.%2C%20Jurasek%2C%20B.%2C%20Sykora%2C%20D.%2C%20Palenicek%2C%20T.%2C%20Miksatkova%2C%20P.%2C%20%26amp%3B%20Kuchar%2C%20M.%20%282015%29.%20Salting-out-assisted%20liquid%26%23x2013%3Bliquid%20extraction%20as%20a%20suitable%20approach%20for%20determination%20of%20methoxetamine%20in%20large%20sets%20of%20tissue%20samples.%20%3Ci%3EAnalytical%20and%20Bioanalytical%20Chemistry%3C%5C%2Fi%3E.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1007%5C%2Fs00216-015-9221-1%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1007%5C%2Fs00216-015-9221-1%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Salting-out-assisted%20liquid%5Cu2013liquid%20extraction%20as%20a%20suitable%20approach%20for%20determination%20of%20methoxetamine%20in%20large%20sets%20of%20tissue%20samples%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Katerina%22%2C%22lastName%22%3A%22Hajkova%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Bronislav%22%2C%22lastName%22%3A%22Jurasek%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22David%22%2C%22lastName%22%3A%22Sykora%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Tomas%22%2C%22lastName%22%3A%22Palenicek%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Petra%22%2C%22lastName%22%3A%22Miksatkova%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Martin%22%2C%22lastName%22%3A%22Kuchar%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222015-12-11%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1007%5C%2Fs00216-015-9221-1%22%2C%22ISSN%22%3A%221618-2642%2C%201618-2650%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Flink.springer.com%5C%2F10.1007%5C%2Fs00216-015-9221-1%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222015-12-30T16%3A26%3A54Z%22%7D%7D%2C%7B%22key%22%3A%22ERQ69KSU%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Wang%20et%20al.%22%2C%22parsedDate%22%3A%222015-12-03%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3EWang%2C%20Y.%2C%20Billon%2C%20C.%2C%20Walker%2C%20J.%20K.%2C%20%26amp%3B%20Burris%2C%20T.%20P.%20%282015%29.%20Therapeutic%20Effect%20of%20a%20Synthetic%20ROR%26%23x3B1%3B%5C%2F%26%23x3B3%3B%20Agonist%20in%20an%20Animal%20Model%20of%20Autism.%20%3Ci%3EACS%20Chemical%20Neuroscience%3C%5C%2Fi%3E.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1021%5C%2Facschemneuro.5b00159%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1021%5C%2Facschemneuro.5b00159%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Therapeutic%20Effect%20of%20a%20Synthetic%20ROR%5Cu03b1%5C%2F%5Cu03b3%20Agonist%20in%20an%20Animal%20Model%20of%20Autism%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Yongjun%22%2C%22lastName%22%3A%22Wang%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Cyrielle%22%2C%22lastName%22%3A%22Billon%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22John%20K.%22%2C%22lastName%22%3A%22Walker%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Thomas%20P.%22%2C%22lastName%22%3A%22Burris%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222015-12-03%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1021%5C%2Facschemneuro.5b00159%22%2C%22ISSN%22%3A%221948-7193%2C%201948-7193%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fpubs.acs.org%5C%2Fdoi%5C%2F10.1021%5C%2Facschemneuro.5b00159%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222015-12-31T20%3A26%3A01Z%22%7D%7D%2C%7B%22key%22%3A%22FGHGQTHE%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Semple%20et%20al.%22%2C%22parsedDate%22%3A%222015-11-20%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3ESemple%2C%20B.%20D.%2C%20Noble-Haeusslein%2C%20L.%20J.%2C%20Gooyit%2C%20M.%2C%20Tercovich%2C%20K.%20G.%2C%20Peng%2C%20Z.%2C%20Nguyen%2C%20T.%20T.%2C%20Schroeder%2C%20V.%20A.%2C%20Suckow%2C%20M.%20A.%2C%20Chang%2C%20M.%2C%20Raber%2C%20J.%2C%20%26amp%3B%20Trivedi%2C%20A.%20%282015%29.%20Early%20Gelatinase%20Activity%20Is%20Not%20a%20Determinant%20of%20Long-Term%20Recovery%20after%20Traumatic%20Brain%20Injury%20in%20the%20Immature%20Mouse.%20%3Ci%3EPLOS%20ONE%3C%5C%2Fi%3E%2C%20%3Ci%3E10%3C%5C%2Fi%3E%2811%29%2C%20e0143386.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1371%5C%2Fjournal.pone.0143386%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1371%5C%2Fjournal.pone.0143386%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Early%20Gelatinase%20Activity%20Is%20Not%20a%20Determinant%20of%20Long-Term%20Recovery%20after%20Traumatic%20Brain%20Injury%20in%20the%20Immature%20Mouse%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Bridgette%20D.%22%2C%22lastName%22%3A%22Semple%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Linda%20J.%22%2C%22lastName%22%3A%22Noble-Haeusslein%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Major%22%2C%22lastName%22%3A%22Gooyit%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Kayleen%20G.%22%2C%22lastName%22%3A%22Tercovich%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Zhihong%22%2C%22lastName%22%3A%22Peng%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Trung%20T.%22%2C%22lastName%22%3A%22Nguyen%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Valerie%20A.%22%2C%22lastName%22%3A%22Schroeder%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Mark%20A.%22%2C%22lastName%22%3A%22Suckow%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Mayland%22%2C%22lastName%22%3A%22Chang%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Jacob%22%2C%22lastName%22%3A%22Raber%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Alpa%22%2C%22lastName%22%3A%22Trivedi%22%7D%2C%7B%22creatorType%22%3A%22editor%22%2C%22firstName%22%3A%22Firas%20H%22%2C%22lastName%22%3A%22Kobeissy%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222015-11-20%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1371%5C%2Fjournal.pone.0143386%22%2C%22ISSN%22%3A%221932-6203%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fdx.plos.org%5C%2F10.1371%5C%2Fjournal.pone.0143386%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222015-12-30T21%3A00%3A44Z%22%7D%7D%2C%7B%22key%22%3A%22EUVQTK9R%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Falendysz%20et%20al.%22%2C%22parsedDate%22%3A%222015-10-30%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3EFalendysz%2C%20E.%20A.%2C%20Lopera%2C%20J.%20G.%2C%20Lorenzsonn%2C%20F.%2C%20Salzer%2C%20J.%20S.%2C%20Hutson%2C%20C.%20L.%2C%20Doty%2C%20J.%2C%20Gallardo-Romero%2C%20N.%2C%20Carroll%2C%20D.%20S.%2C%20Osorio%2C%20J.%20E.%2C%20%26amp%3B%20Rocke%2C%20T.%20E.%20%282015%29.%20Further%20Assessment%20of%20Monkeypox%20Virus%20Infection%20in%20Gambian%20Pouched%20Rats%20%28Cricetomys%20gambianus%29%20Using%20In%20Vivo%20Bioluminescent%20Imaging.%20%3Ci%3EPLOS%20Neglected%20Tropical%20Diseases%3C%5C%2Fi%3E%2C%20%3Ci%3E9%3C%5C%2Fi%3E%2810%29%2C%20e0004130.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1371%5C%2Fjournal.pntd.0004130%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1371%5C%2Fjournal.pntd.0004130%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Further%20Assessment%20of%20Monkeypox%20Virus%20Infection%20in%20Gambian%20Pouched%20Rats%20%28Cricetomys%20gambianus%29%20Using%20In%20Vivo%20Bioluminescent%20Imaging%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Elizabeth%20A.%22%2C%22lastName%22%3A%22Falendysz%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Juan%20G.%22%2C%22lastName%22%3A%22Lopera%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Faye%22%2C%22lastName%22%3A%22Lorenzsonn%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Johanna%20S.%22%2C%22lastName%22%3A%22Salzer%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Christina%20L.%22%2C%22lastName%22%3A%22Hutson%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Jeffrey%22%2C%22lastName%22%3A%22Doty%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Nadia%22%2C%22lastName%22%3A%22Gallardo-Romero%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Darin%20S.%22%2C%22lastName%22%3A%22Carroll%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Jorge%20E.%22%2C%22lastName%22%3A%22Osorio%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Tonie%20E.%22%2C%22lastName%22%3A%22Rocke%22%7D%2C%7B%22creatorType%22%3A%22editor%22%2C%22firstName%22%3A%22A.%20Desiree%22%2C%22lastName%22%3A%22LaBeaud%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222015-10-30%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1371%5C%2Fjournal.pntd.0004130%22%2C%22ISSN%22%3A%221935-2735%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fdx.plos.org%5C%2F10.1371%5C%2Fjournal.pntd.0004130%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222015-12-31T20%3A36%3A31Z%22%7D%7D%2C%7B%22key%22%3A%22932WDIQZ%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Lee%20et%20al.%22%2C%22parsedDate%22%3A%222015-10-21%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3ELee%2C%20M.%2C%20Chen%2C%20Z.%2C%20Tomlinson%2C%20B.%20N.%2C%20Gooyit%2C%20M.%2C%20Hesek%2C%20D.%2C%20Ju%26%23xE1%3Brez%2C%20M.%20R.%2C%20Nizam%2C%20R.%2C%20Boggess%2C%20B.%2C%20Lastochkin%2C%20E.%2C%20Schroeder%2C%20V.%20A.%2C%20Wolter%2C%20W.%20R.%2C%20Suckow%2C%20M.%20A.%2C%20Cui%2C%20J.%2C%20Mobashery%2C%20S.%2C%20Gu%2C%20Z.%2C%20%26amp%3B%20Chang%2C%20M.%20%282015%29.%20Water-Soluble%20MMP-9%20Inhibitor%20Reduces%20Lesion%20Volume%20after%20Severe%20Traumatic%20Brain%20Injury.%20%3Ci%3EACS%20Chemical%20Neuroscience%3C%5C%2Fi%3E%2C%20%3Ci%3E6%3C%5C%2Fi%3E%2810%29%2C%201658%26%23x2013%3B1664.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1021%5C%2Facschemneuro.5b00140%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1021%5C%2Facschemneuro.5b00140%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Water-Soluble%20MMP-9%20Inhibitor%20Reduces%20Lesion%20Volume%20after%20Severe%20Traumatic%20Brain%20Injury%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Mijoon%22%2C%22lastName%22%3A%22Lee%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Zhenzhou%22%2C%22lastName%22%3A%22Chen%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Brittany%20N.%22%2C%22lastName%22%3A%22Tomlinson%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Major%22%2C%22lastName%22%3A%22Gooyit%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Dusan%22%2C%22lastName%22%3A%22Hesek%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Mar%5Cu00eda%20Raquel%22%2C%22lastName%22%3A%22Ju%5Cu00e1rez%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Rasheeq%22%2C%22lastName%22%3A%22Nizam%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Bill%22%2C%22lastName%22%3A%22Boggess%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Elena%22%2C%22lastName%22%3A%22Lastochkin%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Valerie%20A.%22%2C%22lastName%22%3A%22Schroeder%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22William%20R.%22%2C%22lastName%22%3A%22Wolter%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Mark%20A.%22%2C%22lastName%22%3A%22Suckow%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Jiancun%22%2C%22lastName%22%3A%22Cui%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Shahriar%22%2C%22lastName%22%3A%22Mobashery%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Zezong%22%2C%22lastName%22%3A%22Gu%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Mayland%22%2C%22lastName%22%3A%22Chang%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222015-10-21%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1021%5C%2Facschemneuro.5b00140%22%2C%22ISSN%22%3A%221948-7193%2C%201948-7193%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fpubs.acs.org%5C%2Fdoi%5C%2F10.1021%5C%2Facschemneuro.5b00140%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222015-12-31T21%3A22%3A50Z%22%7D%7D%2C%7B%22key%22%3A%22E3X84QV3%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Yau%20et%20al.%22%2C%22parsedDate%22%3A%222015-09-29%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3EYau%2C%20B.%2C%20Mitchell%2C%20A.%20J.%2C%20Too%2C%20L.%20K.%2C%20Ball%2C%20H.%20J.%2C%20%26amp%3B%20Hunt%2C%20N.%20H.%20%282015%29.%20Interferon-%26%23x3B3%3B-Induced%20Nitric%20Oxide%20Synthase-2%20Contributes%20to%20Blood%5C%2FBrain%20Barrier%20Dysfunction%20and%20Acute%20Mortality%20in%20Experimental%20%3Ci%3EStreptococcus%20pneumoniae%3C%5C%2Fi%3E%20Meningitis.%20%3Ci%3EJournal%20of%20Interferon%20%26amp%3B%20Cytokine%20Research%3C%5C%2Fi%3E.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1089%5C%2Fjir.2015.0078%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1089%5C%2Fjir.2015.0078%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Interferon-%5Cu03b3-Induced%20Nitric%20Oxide%20Synthase-2%20Contributes%20to%20Blood%5C%2FBrain%20Barrier%20Dysfunction%20and%20Acute%20Mortality%20in%20Experimental%20%3Ci%3EStreptococcus%20pneumoniae%3C%5C%2Fi%3E%20Meningitis%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Belinda%22%2C%22lastName%22%3A%22Yau%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Andrew%20J.%22%2C%22lastName%22%3A%22Mitchell%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Lay%20Khoon%22%2C%22lastName%22%3A%22Too%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Helen%20J.%22%2C%22lastName%22%3A%22Ball%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Nicholas%20H.%22%2C%22lastName%22%3A%22Hunt%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222015-09-29%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1089%5C%2Fjir.2015.0078%22%2C%22ISSN%22%3A%221079-9907%2C%201557-7465%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fonline.liebertpub.com%5C%2Fdoi%5C%2F10.1089%5C%2Fjir.2015.0078%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222015-12-31T18%3A11%3A05Z%22%7D%7D%2C%7B%22key%22%3A%22R3NHG865%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Crowell%20et%20al.%22%2C%22parsedDate%22%3A%222015-08-05%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3ECrowell%2C%20J.%2C%20Hughson%2C%20A.%2C%20Caughey%2C%20B.%2C%20%26amp%3B%20Bessen%2C%20R.%20A.%20%282015%29.%20Host%20determinants%20of%20prion%20strain%20diversity%20independent%20of%20prion%20protein%20genotype.%20%3Ci%3EJournal%20of%20Virology%3C%5C%2Fi%3E%2C%20JVI.01586-15.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1128%5C%2FJVI.01586-15%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1128%5C%2FJVI.01586-15%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Host%20determinants%20of%20prion%20strain%20diversity%20independent%20of%20prion%20protein%20genotype%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Jenna%22%2C%22lastName%22%3A%22Crowell%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Andrew%22%2C%22lastName%22%3A%22Hughson%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Byron%22%2C%22lastName%22%3A%22Caughey%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Richard%20A.%22%2C%22lastName%22%3A%22Bessen%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222015-08-05%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1128%5C%2FJVI.01586-15%22%2C%22ISSN%22%3A%220022-538X%2C%201098-5514%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fjvi.asm.org%5C%2Flookup%5C%2Fdoi%5C%2F10.1128%5C%2FJVI.01586-15%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222015-08-12T16%3A41%3A45Z%22%7D%7D%2C%7B%22key%22%3A%22562DWGEC%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Xu%20et%20al.%22%2C%22parsedDate%22%3A%222015-06-22%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3EXu%2C%20X.-F.%2C%20Li%2C%20T.%2C%20Wang%2C%20D.-D.%2C%20Chen%2C%20B.%2C%20Wang%2C%20Y.%2C%20%26amp%3B%20Chen%2C%20Z.-Y.%20%282015%29.%20Integrin-linked%20Kinase%20is%20Essential%20for%20Environmental%20Enrichment%20Enhanced%20Hippocampal%20Neurogenesis%20and%20Memory.%20%3Ci%3EScientific%20Reports%3C%5C%2Fi%3E%2C%20%3Ci%3E5%3C%5C%2Fi%3E%2C%2011456.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1038%5C%2Fsrep11456%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1038%5C%2Fsrep11456%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Integrin-linked%20Kinase%20is%20Essential%20for%20Environmental%20Enrichment%20Enhanced%20Hippocampal%20Neurogenesis%20and%20Memory%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Xu-Feng%22%2C%22lastName%22%3A%22Xu%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Ting%22%2C%22lastName%22%3A%22Li%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Dong-Dong%22%2C%22lastName%22%3A%22Wang%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Bing%22%2C%22lastName%22%3A%22Chen%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Yue%22%2C%22lastName%22%3A%22Wang%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Zhe-Yu%22%2C%22lastName%22%3A%22Chen%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222015-6-22%22%2C%22language%22%3A%22%22%2C%22DOI%22%3A%2210.1038%5C%2Fsrep11456%22%2C%22ISSN%22%3A%222045-2322%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fwww.nature.com%5C%2Farticles%5C%2Fsrep11456%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222015-12-31T20%3A53%3A57Z%22%7D%7D%2C%7B%22key%22%3A%22CDKJ6W8V%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Grasso%20et%20al.%22%2C%22parsedDate%22%3A%222015-05-04%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3EGrasso%2C%20C.%20S.%2C%20Tang%2C%20Y.%2C%20Truffaux%2C%20N.%2C%20Berlow%2C%20N.%20E.%2C%20Liu%2C%20L.%2C%20Debily%2C%20M.-A.%2C%20Quist%2C%20M.%20J.%2C%20Davis%2C%20L.%20E.%2C%20Huang%2C%20E.%20C.%2C%20Woo%2C%20P.%20J.%2C%20Ponnuswami%2C%20A.%2C%20Chen%2C%20S.%2C%20Johung%2C%20T.%20B.%2C%20Sun%2C%20W.%2C%20Kogiso%2C%20M.%2C%20Du%2C%20Y.%2C%20Qi%2C%20L.%2C%20Huang%2C%20Y.%2C%20H%26%23xFC%3Btt-Cabezas%2C%20M.%2C%20%26%23x2026%3B%20Monje%2C%20M.%20%282015%29.%20Functionally%20defined%20therapeutic%20targets%20in%20diffuse%20intrinsic%20pontine%20glioma.%20%3Ci%3ENature%20Medicine%3C%5C%2Fi%3E%2C%20%3Ci%3E21%3C%5C%2Fi%3E%286%29%2C%20555%26%23x2013%3B559.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1038%5C%2Fnm.3855%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1038%5C%2Fnm.3855%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Functionally%20defined%20therapeutic%20targets%20in%20diffuse%20intrinsic%20pontine%20glioma%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Catherine%20S%22%2C%22lastName%22%3A%22Grasso%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Yujie%22%2C%22lastName%22%3A%22Tang%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Nathalene%22%2C%22lastName%22%3A%22Truffaux%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Noah%20E%22%2C%22lastName%22%3A%22Berlow%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Lining%22%2C%22lastName%22%3A%22Liu%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Marie-Anne%22%2C%22lastName%22%3A%22Debily%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Michael%20J%22%2C%22lastName%22%3A%22Quist%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Lara%20E%22%2C%22lastName%22%3A%22Davis%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Elaine%20C%22%2C%22lastName%22%3A%22Huang%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Pamelyn%20J%22%2C%22lastName%22%3A%22Woo%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Anitha%22%2C%22lastName%22%3A%22Ponnuswami%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Spenser%22%2C%22lastName%22%3A%22Chen%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Tessa%20B%22%2C%22lastName%22%3A%22Johung%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Wenchao%22%2C%22lastName%22%3A%22Sun%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Mari%22%2C%22lastName%22%3A%22Kogiso%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Yuchen%22%2C%22lastName%22%3A%22Du%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Lin%22%2C%22lastName%22%3A%22Qi%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Yulun%22%2C%22lastName%22%3A%22Huang%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Marianne%22%2C%22lastName%22%3A%22H%5Cu00fctt-Cabezas%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Katherine%20E%22%2C%22lastName%22%3A%22Warren%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Ludivine%22%2C%22lastName%22%3A%22Le%20Dret%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Paul%20S%22%2C%22lastName%22%3A%22Meltzer%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Hua%22%2C%22lastName%22%3A%22Mao%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Martha%22%2C%22lastName%22%3A%22Quezado%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Dannis%20G%22%2C%22lastName%22%3A%22van%20Vuurden%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Jinu%22%2C%22lastName%22%3A%22Abraham%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Maryam%22%2C%22lastName%22%3A%22Fouladi%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Matthew%20N%22%2C%22lastName%22%3A%22Svalina%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Nicholas%22%2C%22lastName%22%3A%22Wang%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Cynthia%22%2C%22lastName%22%3A%22Hawkins%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Javad%22%2C%22lastName%22%3A%22Nazarian%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Marta%20M%22%2C%22lastName%22%3A%22Alonso%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Eric%20H%22%2C%22lastName%22%3A%22Raabe%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Esther%22%2C%22lastName%22%3A%22Hulleman%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Paul%20T%22%2C%22lastName%22%3A%22Spellman%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Xiao-Nan%22%2C%22lastName%22%3A%22Li%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Charles%22%2C%22lastName%22%3A%22Keller%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Ranadip%22%2C%22lastName%22%3A%22Pal%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Jacques%22%2C%22lastName%22%3A%22Grill%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Michelle%22%2C%22lastName%22%3A%22Monje%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222015-5-4%22%2C%22language%22%3A%22%22%2C%22DOI%22%3A%2210.1038%5C%2Fnm.3855%22%2C%22ISSN%22%3A%221078-8956%2C%201546-170X%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fwww.nature.com%5C%2Fdoifinder%5C%2F10.1038%5C%2Fnm.3855%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222015-08-03T15%3A21%3A09Z%22%7D%7D%2C%7B%22key%22%3A%22A63PZ65J%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Ciesielska%20et%20al.%22%2C%22parsedDate%22%3A%222015-04-10%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3ECiesielska%2C%20A.%2C%20Sharma%2C%20N.%2C%20Beyer%2C%20J.%2C%20Forsayeth%2C%20J.%2C%20%26amp%3B%20Bankiewicz%2C%20K.%20%282015%29.%20Carbidopa-Based%20Modulation%20of%20the%20Functional%20Effect%20of%20the%20AAV2-hAADC%20Gene%20Therapy%20in%206-OHDA%20Lesioned%20Rats.%20%3Ci%3EPLOS%20ONE%3C%5C%2Fi%3E%2C%20%3Ci%3E10%3C%5C%2Fi%3E%284%29%2C%20e0122708.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1371%5C%2Fjournal.pone.0122708%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1371%5C%2Fjournal.pone.0122708%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Carbidopa-Based%20Modulation%20of%20the%20Functional%20Effect%20of%20the%20AAV2-hAADC%20Gene%20Therapy%20in%206-OHDA%20Lesioned%20Rats%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Agnieszka%22%2C%22lastName%22%3A%22Ciesielska%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Nitasha%22%2C%22lastName%22%3A%22Sharma%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Janine%22%2C%22lastName%22%3A%22Beyer%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22John%22%2C%22lastName%22%3A%22Forsayeth%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Krystof%22%2C%22lastName%22%3A%22Bankiewicz%22%7D%2C%7B%22creatorType%22%3A%22editor%22%2C%22firstName%22%3A%22Joohyung%22%2C%22lastName%22%3A%22Lee%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222015-4-10%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1371%5C%2Fjournal.pone.0122708%22%2C%22ISSN%22%3A%221932-6203%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fdx.plos.org%5C%2F10.1371%5C%2Fjournal.pone.0122708%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222015-10-30T20%3A52%3A22Z%22%7D%7D%2C%7B%22key%22%3A%22UZ5U957H%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Crowell%20et%20al.%22%2C%22parsedDate%22%3A%222015-03-30%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3ECrowell%2C%20J.%2C%20Wiley%2C%20J.%20A.%2C%20%26amp%3B%20Bessen%2C%20R.%20A.%20%282015%29.%20Lesion%20of%20the%20Olfactory%20Epithelium%20Accelerates%20Prion%20Neuroinvasion%20and%20Disease%20Onset%20when%20Prion%20Replication%20Is%20Restricted%20to%20Neurons.%20%3Ci%3EPLOS%20ONE%3C%5C%2Fi%3E%2C%20%3Ci%3E10%3C%5C%2Fi%3E%283%29%2C%20e0119863.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1371%5C%2Fjournal.pone.0119863%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1371%5C%2Fjournal.pone.0119863%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Lesion%20of%20the%20Olfactory%20Epithelium%20Accelerates%20Prion%20Neuroinvasion%20and%20Disease%20Onset%20when%20Prion%20Replication%20Is%20Restricted%20to%20Neurons%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Jenna%22%2C%22lastName%22%3A%22Crowell%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22James%20A.%22%2C%22lastName%22%3A%22Wiley%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Richard%20A.%22%2C%22lastName%22%3A%22Bessen%22%7D%2C%7B%22creatorType%22%3A%22editor%22%2C%22firstName%22%3A%22Gianluigi%22%2C%22lastName%22%3A%22Zanusso%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222015-3-30%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1371%5C%2Fjournal.pone.0119863%22%2C%22ISSN%22%3A%221932-6203%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fdx.plos.org%5C%2F10.1371%5C%2Fjournal.pone.0119863%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222015-08-06T16%3A39%3A30Z%22%7D%7D%2C%7B%22key%22%3A%22HPCWHGBQ%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Wang%20et%20al.%22%2C%22parsedDate%22%3A%222015-02-06%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3EWang%2C%20H.%2C%20Yang%2C%20Y.%2C%20Li%2C%20Y.%2C%20Bai%2C%20B.%2C%20Wang%2C%20X.%2C%20Tan%2C%20H.%2C%20Liu%2C%20T.%2C%20Beach%2C%20T.%20G.%2C%20Peng%2C%20J.%2C%20%26amp%3B%20Wu%2C%20Z.%20%282015%29.%20Systematic%20Optimization%20of%20Long%20Gradient%20Chromatography%20Mass%20Spectrometry%20for%20Deep%20Analysis%20of%20Brain%20Proteome.%20%3Ci%3EJournal%20of%20Proteome%20Research%3C%5C%2Fi%3E%2C%20%3Ci%3E14%3C%5C%2Fi%3E%282%29%2C%20829%26%23x2013%3B838.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1021%5C%2Fpr500882h%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1021%5C%2Fpr500882h%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Systematic%20Optimization%20of%20Long%20Gradient%20Chromatography%20Mass%20Spectrometry%20for%20Deep%20Analysis%20of%20Brain%20Proteome%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Hong%22%2C%22lastName%22%3A%22Wang%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Yanling%22%2C%22lastName%22%3A%22Yang%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Yuxin%22%2C%22lastName%22%3A%22Li%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Bing%22%2C%22lastName%22%3A%22Bai%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Xusheng%22%2C%22lastName%22%3A%22Wang%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Haiyan%22%2C%22lastName%22%3A%22Tan%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Tao%22%2C%22lastName%22%3A%22Liu%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Thomas%20G.%22%2C%22lastName%22%3A%22Beach%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Junmin%22%2C%22lastName%22%3A%22Peng%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Zhiping%22%2C%22lastName%22%3A%22Wu%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222015-02-06%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1021%5C%2Fpr500882h%22%2C%22ISSN%22%3A%221535-3893%2C%201535-3907%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fpubs.acs.org%5C%2Fdoi%5C%2Fabs%5C%2F10.1021%5C%2Fpr500882h%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222015-10-29T21%3A24%3A15Z%22%7D%7D%2C%7B%22key%22%3A%22WZBGX7B9%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Burrell-Saward%22%2C%22parsedDate%22%3A%222015-01%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3EBurrell-Saward%2C%20H.%20%282015%29.%20%3Ci%3EDevelopment%20of%20an%20imaging%20model%20of%20a%20CNS%20infection%20with%20African%20trypanosomes.%3C%5C%2Fi%3E%20%5BLondon%20School%20of%20Hygeine%20and%20Tropical%20Medicine%5D.%20%3Ca%20class%3D%27zp-ItemURL%27%20href%3D%27http%3A%5C%2F%5C%2Fresearchonline.lshtm.ac.uk%5C%2F2222110%5C%2F1%5C%2F2015_ITD_PhD_Burrell-Saward_H.pdf%27%3Ehttp%3A%5C%2F%5C%2Fresearchonline.lshtm.ac.uk%5C%2F2222110%5C%2F1%5C%2F2015_ITD_PhD_Burrell-Saward_H.pdf%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22thesis%22%2C%22title%22%3A%22Development%20of%20an%20imaging%20model%20of%20a%20CNS%20infection%20with%20African%20trypanosomes.%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Hollie%22%2C%22lastName%22%3A%22Burrell-Saward%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22thesisType%22%3A%22%22%2C%22university%22%3A%22London%20School%20of%20Hygeine%20and%20Tropical%20Medicine%22%2C%22date%22%3A%22January%202015%22%2C%22language%22%3A%22%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fresearchonline.lshtm.ac.uk%5C%2F2222110%5C%2F1%5C%2F2015_ITD_PhD_Burrell-Saward_H.pdf%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222016-01-11T21%3A14%3A18Z%22%7D%7D%2C%7B%22key%22%3A%22ZRNHIZRV%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Evers%20et%20al.%22%2C%22parsedDate%22%3A%222015%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3EEvers%2C%20M.%20M.%2C%20Schut%2C%20M.%20H.%2C%20Pepers%2C%20B.%20A.%2C%20Atalar%2C%20M.%2C%20van%20Belzen%2C%20M.%20J.%2C%20Faull%2C%20R.%20L.%2C%20Roos%2C%20R.%20A.%2C%20%26amp%3B%20van%20Roon-Mom%2C%20W.%20M.%20%282015%29.%20Making%20%28anti-%29%20sense%20out%20of%20huntingtin%20levels%20in%20Huntington%20disease.%20%3Ci%3EMolecular%20Neurodegeneration%3C%5C%2Fi%3E%2C%20%3Ci%3E10%3C%5C%2Fi%3E%281%29.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1186%5C%2Fs13024-015-0018-7%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1186%5C%2Fs13024-015-0018-7%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Making%20%28anti-%29%20sense%20out%20of%20huntingtin%20levels%20in%20Huntington%20disease%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Melvin%20M%22%2C%22lastName%22%3A%22Evers%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Menno%20H%22%2C%22lastName%22%3A%22Schut%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Barry%20A%22%2C%22lastName%22%3A%22Pepers%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Melek%22%2C%22lastName%22%3A%22Atalar%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Martine%20J%22%2C%22lastName%22%3A%22van%20Belzen%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Richard%20LM%22%2C%22lastName%22%3A%22Faull%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Raymund%20AC%22%2C%22lastName%22%3A%22Roos%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Willeke%20MC%22%2C%22lastName%22%3A%22van%20Roon-Mom%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%2212%5C%2F2015%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1186%5C%2Fs13024-015-0018-7%22%2C%22ISSN%22%3A%221750-1326%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fwww.molecularneurodegeneration.com%5C%2Fcontent%5C%2F10%5C%2F1%5C%2F21%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222015-12-30T21%3A30%3A28Z%22%7D%7D%2C%7B%22key%22%3A%22NUGCIXQF%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Doldur-Balli%20et%20al.%22%2C%22parsedDate%22%3A%222015%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3EDoldur-Balli%2C%20F.%2C%20Ozel%2C%20M.%20N.%2C%20Gulsuner%2C%20S.%2C%20Tekinay%2C%20A.%20B.%2C%20Ozcelik%2C%20T.%2C%20Konu%2C%20O.%2C%20%26amp%3B%20Adams%2C%20M.%20M.%20%282015%29.%20Characterization%20of%20a%20novel%20zebrafish%20%28Danio%20rerio%29%20gene%2C%20wdr81%2C%20associated%20with%20cerebellar%20ataxia%2C%20mental%20retardation%20and%20dysequilibrium%20syndrome%20%28CAMRQ%29.%20%3Ci%3EBMC%20Neuroscience%3C%5C%2Fi%3E%2C%20%3Ci%3E16%3C%5C%2Fi%3E%281%29.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1186%5C%2Fs12868-015-0229-4%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1186%5C%2Fs12868-015-0229-4%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Characterization%20of%20a%20novel%20zebrafish%20%28Danio%20rerio%29%20gene%2C%20wdr81%2C%20associated%20with%20cerebellar%20ataxia%2C%20mental%20retardation%20and%20dysequilibrium%20syndrome%20%28CAMRQ%29%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Fusun%22%2C%22lastName%22%3A%22Doldur-Balli%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Mehmet%20Neset%22%2C%22lastName%22%3A%22Ozel%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Suleyman%22%2C%22lastName%22%3A%22Gulsuner%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Ayse%20B.%22%2C%22lastName%22%3A%22Tekinay%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Tayfun%22%2C%22lastName%22%3A%22Ozcelik%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Ozlen%22%2C%22lastName%22%3A%22Konu%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Michelle%20M.%22%2C%22lastName%22%3A%22Adams%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%2212%5C%2F2015%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1186%5C%2Fs12868-015-0229-4%22%2C%22ISSN%22%3A%221471-2202%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fwww.biomedcentral.com%5C%2F1471-2202%5C%2F16%5C%2F96%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222015-12-30T18%3A54%3A48Z%22%7D%7D%2C%7B%22key%22%3A%223PV3DF32%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Kumar%20et%20al.%22%2C%22parsedDate%22%3A%222015%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3EKumar%2C%20M.%2C%20Roe%2C%20K.%2C%20O%26%23x2019%3BConnell%2C%20M.%2C%20%26amp%3B%20Nerurkar%2C%20V.%20R.%20%282015%29.%20Induction%20of%20virus-specific%20effector%20immune%20cell%20response%20limits%20virus%20replication%20and%20severe%20disease%20in%20mice%20infected%20with%20non-lethal%20West%20Nile%20virus%20Eg101%20strain.%20%3Ci%3EJournal%20of%20Neuroinflammation%3C%5C%2Fi%3E%2C%20%3Ci%3E12%3C%5C%2Fi%3E%281%29.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1186%5C%2Fs12974-015-0400-y%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1186%5C%2Fs12974-015-0400-y%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Induction%20of%20virus-specific%20effector%20immune%20cell%20response%20limits%20virus%20replication%20and%20severe%20disease%20in%20mice%20infected%20with%20non-lethal%20West%20Nile%20virus%20Eg101%20strain%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Mukesh%22%2C%22lastName%22%3A%22Kumar%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Kelsey%22%2C%22lastName%22%3A%22Roe%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Maile%22%2C%22lastName%22%3A%22O%5Cu2019Connell%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Vivek%20R.%22%2C%22lastName%22%3A%22Nerurkar%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%2212%5C%2F2015%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1186%5C%2Fs12974-015-0400-y%22%2C%22ISSN%22%3A%221742-2094%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fwww.jneuroinflammation.com%5C%2Fcontent%5C%2F12%5C%2F1%5C%2F178%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222015-12-30T18%3A50%3A30Z%22%7D%7D%2C%7B%22key%22%3A%224VURJJ6Q%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Khademi%20et%20al.%22%2C%22parsedDate%22%3A%222015%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3EKhademi%2C%20S.%2C%20Frye%2C%20M.%20A.%2C%20Jeckel%2C%20K.%20M.%2C%20Schroeder%2C%20T.%2C%20Monnet%2C%20E.%2C%20Irwin%2C%20D.%20C.%2C%20Cole%2C%20P.%20A.%2C%20Bell%2C%20C.%2C%20Miller%2C%20B.%20F.%2C%20%26amp%3B%20Hamilton%2C%20K.%20L.%20%282015%29.%20Hypoxia%20mediated%20pulmonary%20edema%3A%20potential%20influence%20of%20oxidative%20stress%2C%20sympathetic%20activation%20and%20cerebral%20blood%20flow.%20%3Ci%3EBMC%20Physiology%3C%5C%2Fi%3E%2C%20%3Ci%3E15%3C%5C%2Fi%3E%281%29.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1186%5C%2Fs12899-015-0018-4%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1186%5C%2Fs12899-015-0018-4%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Hypoxia%20mediated%20pulmonary%20edema%3A%20potential%20influence%20of%20oxidative%20stress%2C%20sympathetic%20activation%20and%20cerebral%20blood%20flow%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Shadi%22%2C%22lastName%22%3A%22Khademi%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Melinda%20A.%22%2C%22lastName%22%3A%22Frye%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Kimberly%20M.%22%2C%22lastName%22%3A%22Jeckel%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Thies%22%2C%22lastName%22%3A%22Schroeder%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Eric%22%2C%22lastName%22%3A%22Monnet%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Dave%20C.%22%2C%22lastName%22%3A%22Irwin%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Patricia%20A.%22%2C%22lastName%22%3A%22Cole%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Christopher%22%2C%22lastName%22%3A%22Bell%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Benjamin%20F.%22%2C%22lastName%22%3A%22Miller%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Karyn%20L.%22%2C%22lastName%22%3A%22Hamilton%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%2212%5C%2F2015%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1186%5C%2Fs12899-015-0018-4%22%2C%22ISSN%22%3A%221472-6793%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fwww.biomedcentral.com%5C%2F1472-6793%5C%2F15%5C%2F4%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222015-10-30T13%3A21%3A43Z%22%7D%7D%2C%7B%22key%22%3A%22WXHNMTHH%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Yuan%20and%20Rapoport%22%2C%22parsedDate%22%3A%222015%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3EYuan%2C%20Z.-X.%2C%20%26amp%3B%20Rapoport%2C%20S.%20I.%20%282015%29.%20Transient%20postnatal%20fluoxetine%20decreases%20brain%20concentrations%20of%2020-HETE%20and%2015-epi-LXA4%2C%20arachidonic%20acid%20metabolites%20in%20adult%20mice.%20%3Ci%3EProstaglandins%2C%20Leukotrienes%20and%20Essential%20Fatty%20Acids%20%28PLEFA%29%3C%5C%2Fi%3E%2C%20%3Ci%3E101%3C%5C%2Fi%3E%2C%209%26%23x2013%3B14.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2Fj.plefa.2015.07.002%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2Fj.plefa.2015.07.002%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Transient%20postnatal%20fluoxetine%20decreases%20brain%20concentrations%20of%2020-HETE%20and%2015-epi-LXA4%2C%20arachidonic%20acid%20metabolites%20in%20adult%20mice%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Zhi-Xin%22%2C%22lastName%22%3A%22Yuan%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Stanley%20I.%22%2C%22lastName%22%3A%22Rapoport%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%2210%5C%2F2015%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1016%5C%2Fj.plefa.2015.07.002%22%2C%22ISSN%22%3A%2209523278%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Flinkinghub.elsevier.com%5C%2Fretrieve%5C%2Fpii%5C%2FS0952327815001362%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222015-12-30T19%3A03%3A44Z%22%7D%7D%2C%7B%22key%22%3A%22M34F2TNK%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Wong%20and%20Godwin%22%2C%22parsedDate%22%3A%222015%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3EWong%2C%20R.%20Y.%2C%20%26amp%3B%20Godwin%2C%20J.%20%282015%29.%20Neurotranscriptome%20profiles%20of%20multiple%20zebrafish%20strains.%20%3Ci%3EGenomics%20Data%3C%5C%2Fi%3E%2C%20%3Ci%3E5%3C%5C%2Fi%3E%2C%20206%26%23x2013%3B209.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2Fj.gdata.2015.06.004%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2Fj.gdata.2015.06.004%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Neurotranscriptome%20profiles%20of%20multiple%20zebrafish%20strains%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Ryan%20Y.%22%2C%22lastName%22%3A%22Wong%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22John%22%2C%22lastName%22%3A%22Godwin%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%2209%5C%2F2015%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1016%5C%2Fj.gdata.2015.06.004%22%2C%22ISSN%22%3A%2222135960%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Flinkinghub.elsevier.com%5C%2Fretrieve%5C%2Fpii%5C%2FS2213596015001051%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222015-08-03T14%3A24%3A43Z%22%7D%7D%2C%7B%22key%22%3A%22MBSU9NWF%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Hallgren%20et%20al.%22%2C%22parsedDate%22%3A%222015%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3EHallgren%2C%20S.%2C%20Fredriksson%2C%20A.%2C%20%26amp%3B%20Viberg%2C%20H.%20%282015%29.%20More%20signs%20of%20neurotoxicity%20of%20surfactants%20and%20flame%20retardants%20%26%23x2013%3B%20Neonatal%20PFOS%20and%20PBDE%2099%20cause%20transcriptional%20alterations%20in%20cholinergic%20genes%20in%20the%20mouse%20CNS.%20%3Ci%3EEnvironmental%20Toxicology%20and%20Pharmacology%3C%5C%2Fi%3E%2C%20%3Ci%3E40%3C%5C%2Fi%3E%282%29%2C%20409%26%23x2013%3B416.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2Fj.etap.2015.06.014%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2Fj.etap.2015.06.014%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22More%20signs%20of%20neurotoxicity%20of%20surfactants%20and%20flame%20retardants%20%5Cu2013%20Neonatal%20PFOS%20and%20PBDE%2099%20cause%20transcriptional%20alterations%20in%20cholinergic%20genes%20in%20the%20mouse%20CNS%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Stefan%22%2C%22lastName%22%3A%22Hallgren%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Anders%22%2C%22lastName%22%3A%22Fredriksson%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Henrik%22%2C%22lastName%22%3A%22Viberg%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%2209%5C%2F2015%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1016%5C%2Fj.etap.2015.06.014%22%2C%22ISSN%22%3A%2213826689%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Flinkinghub.elsevier.com%5C%2Fretrieve%5C%2Fpii%5C%2FS1382668915300144%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222015-10-30T19%3A55%3A08Z%22%7D%7D%2C%7B%22key%22%3A%22VGJ4K52X%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Zhou%20et%20al.%22%2C%22parsedDate%22%3A%222015%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3EZhou%2C%20J.%2C%20Coles%2C%20L.%20D.%2C%20Kartha%2C%20R.%20V.%2C%20Nash%2C%20N.%2C%20Mishra%2C%20U.%2C%20Lund%2C%20T.%20C.%2C%20%26amp%3B%20Cloyd%2C%20J.%20C.%20%282015%29.%20Intravenous%20Administration%20of%20Stable-Labeled%20N-Acetylcysteine%20Demonstrates%20an%20Indirect%20Mechanism%20for%20Boosting%20Glutathione%20and%20Improving%20Redox%20Status.%20%3Ci%3EJournal%20of%20Pharmaceutical%20Sciences%3C%5C%2Fi%3E%2C%20%3Ci%3E104%3C%5C%2Fi%3E%288%29%2C%202619%26%23x2013%3B2626.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1002%5C%2Fjps.24482%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1002%5C%2Fjps.24482%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Intravenous%20Administration%20of%20Stable-Labeled%20N-Acetylcysteine%20Demonstrates%20an%20Indirect%20Mechanism%20for%20Boosting%20Glutathione%20and%20Improving%20Redox%20Status%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Jie%22%2C%22lastName%22%3A%22Zhou%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Lisa%20D.%22%2C%22lastName%22%3A%22Coles%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Reena%20V.%22%2C%22lastName%22%3A%22Kartha%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Nardina%22%2C%22lastName%22%3A%22Nash%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Usha%22%2C%22lastName%22%3A%22Mishra%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Troy%20C.%22%2C%22lastName%22%3A%22Lund%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22James%20C.%22%2C%22lastName%22%3A%22Cloyd%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%2208%5C%2F2015%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1002%5C%2Fjps.24482%22%2C%22ISSN%22%3A%2200223549%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fdoi.wiley.com%5C%2F10.1002%5C%2Fjps.24482%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222015-12-30T20%3A45%3A09Z%22%7D%7D%2C%7B%22key%22%3A%223HBQWMPI%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Razafsky%20and%20Hodzic%22%2C%22parsedDate%22%3A%222015%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3ERazafsky%2C%20D.%2C%20%26amp%3B%20Hodzic%2C%20D.%20%282015%29.%20A%20variant%20of%20Nesprin1%20giant%20devoid%20of%20KASH%20domain%20underlies%20the%20molecular%20etiology%20of%20autosomal%20recessive%20cerebellar%20ataxia%20type%20I.%20%3Ci%3ENeurobiology%20of%20Disease%3C%5C%2Fi%3E%2C%20%3Ci%3E78%3C%5C%2Fi%3E%2C%2057%26%23x2013%3B67.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2Fj.nbd.2015.03.027%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2Fj.nbd.2015.03.027%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22A%20variant%20of%20Nesprin1%20giant%20devoid%20of%20KASH%20domain%20underlies%20the%20molecular%20etiology%20of%20autosomal%20recessive%20cerebellar%20ataxia%20type%20I%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22David%22%2C%22lastName%22%3A%22Razafsky%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Didier%22%2C%22lastName%22%3A%22Hodzic%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%2206%5C%2F2015%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1016%5C%2Fj.nbd.2015.03.027%22%2C%22ISSN%22%3A%2209699961%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Flinkinghub.elsevier.com%5C%2Fretrieve%5C%2Fpii%5C%2FS0969996115001059%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222015-07-31T15%3A28%3A45Z%22%7D%7D%2C%7B%22key%22%3A%225QZU7HZE%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Aryal%20et%20al.%22%2C%22parsedDate%22%3A%222015%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3EAryal%2C%20M.%2C%20Vykhodtseva%2C%20N.%2C%20Zhang%2C%20Y.-Z.%2C%20%26amp%3B%20McDannold%2C%20N.%20%282015%29.%20Multiple%20sessions%20of%20liposomal%20doxorubicin%20delivery%20via%20focused%20ultrasound%20mediated%20blood%26%23x2013%3Bbrain%20barrier%20disruption%3A%20A%20safety%20study.%20%3Ci%3EJournal%20of%20Controlled%20Release%3C%5C%2Fi%3E%2C%20%3Ci%3E204%3C%5C%2Fi%3E%2C%2060%26%23x2013%3B69.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2Fj.jconrel.2015.02.033%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2Fj.jconrel.2015.02.033%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Multiple%20sessions%20of%20liposomal%20doxorubicin%20delivery%20via%20focused%20ultrasound%20mediated%20blood%5Cu2013brain%20barrier%20disruption%3A%20A%20safety%20study%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Muna%22%2C%22lastName%22%3A%22Aryal%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Natalia%22%2C%22lastName%22%3A%22Vykhodtseva%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Yong-Zhi%22%2C%22lastName%22%3A%22Zhang%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Nathan%22%2C%22lastName%22%3A%22McDannold%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%2204%5C%2F2015%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1016%5C%2Fj.jconrel.2015.02.033%22%2C%22ISSN%22%3A%2201683659%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Flinkinghub.elsevier.com%5C%2Fretrieve%5C%2Fpii%5C%2FS0168365915001431%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222015-12-31T19%3A52%3A23Z%22%7D%7D%2C%7B%22key%22%3A%22VZ8DQ7ST%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22H%5Cu00e4gglund%20et%20al.%22%2C%22parsedDate%22%3A%222015%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3EH%26%23xE4%3Bgglund%2C%20M.%20G.%20A.%2C%20Hellsten%2C%20S.%20V.%2C%20Bagchi%2C%20S.%2C%20Philippot%2C%20G.%2C%20L%26%23xF6%3Bfqvist%2C%20E.%2C%20Nilsson%2C%20V.%20C.%20O.%2C%20Almkvist%2C%20I.%2C%20Karlsson%2C%20E.%2C%20Sreedharan%2C%20S.%2C%20Tafreshiha%2C%20A.%2C%20%26amp%3B%20Fredriksson%2C%20R.%20%282015%29.%20Transport%20of%20l-Glutamine%2C%20l-Alanine%2C%20l-Arginine%20and%20l-Histidine%20by%20the%20Neuron-Specific%20Slc38a8%20%28SNAT8%29%20in%20CNS.%20%3Ci%3EJournal%20of%20Molecular%20Biology%3C%5C%2Fi%3E%2C%20%3Ci%3E427%3C%5C%2Fi%3E%286%29%2C%201495%26%23x2013%3B1512.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2Fj.jmb.2014.10.016%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1016%5C%2Fj.jmb.2014.10.016%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Transport%20of%20l-Glutamine%2C%20l-Alanine%2C%20l-Arginine%20and%20l-Histidine%20by%20the%20Neuron-Specific%20Slc38a8%20%28SNAT8%29%20in%20CNS%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Maria%20G.A.%22%2C%22lastName%22%3A%22H%5Cu00e4gglund%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Sofie%20V.%22%2C%22lastName%22%3A%22Hellsten%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Sonchita%22%2C%22lastName%22%3A%22Bagchi%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Ga%5Cu00ebtan%22%2C%22lastName%22%3A%22Philippot%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Erik%22%2C%22lastName%22%3A%22L%5Cu00f6fqvist%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Victor%20C.O.%22%2C%22lastName%22%3A%22Nilsson%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Ingrid%22%2C%22lastName%22%3A%22Almkvist%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Edvin%22%2C%22lastName%22%3A%22Karlsson%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Smitha%22%2C%22lastName%22%3A%22Sreedharan%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Atieh%22%2C%22lastName%22%3A%22Tafreshiha%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Robert%22%2C%22lastName%22%3A%22Fredriksson%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%2203%5C%2F2015%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1016%5C%2Fj.jmb.2014.10.016%22%2C%22ISSN%22%3A%2200222836%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Flinkinghub.elsevier.com%5C%2Fretrieve%5C%2Fpii%5C%2FS0022283614005671%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222016-01-04T22%3A04%3A06Z%22%7D%7D%2C%7B%22key%22%3A%2287GSV4K5%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Drew%20et%20al.%22%2C%22parsedDate%22%3A%222015%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3EDrew%2C%20P.%20D.%2C%20Johnson%2C%20J.%20W.%2C%20Douglas%2C%20J.%20C.%2C%20Phelan%2C%20K.%20D.%2C%20%26amp%3B%20Kane%2C%20C.%20J.%20M.%20%282015%29.%20Pioglitazone%20Blocks%20Ethanol%20Induction%20of%20Microglial%20Activation%20and%20Immune%20Responses%20in%20the%20Hippocampus%2C%20Cerebellum%2C%20and%20Cerebral%20Cortex%20in%20a%20Mouse%20Model%20of%20Fetal%20Alcohol%20Spectrum%20Disorders.%20%3Ci%3EAlcoholism%3A%20Clinical%20and%20Experimental%20Research%3C%5C%2Fi%3E%2C%20%3Ci%3E39%3C%5C%2Fi%3E%283%29%2C%20445%26%23x2013%3B454.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1111%5C%2Facer.12639%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1111%5C%2Facer.12639%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Pioglitazone%20Blocks%20Ethanol%20Induction%20of%20Microglial%20Activation%20and%20Immune%20Responses%20in%20the%20Hippocampus%2C%20Cerebellum%2C%20and%20Cerebral%20Cortex%20in%20a%20Mouse%20Model%20of%20Fetal%20Alcohol%20Spectrum%20Disorders%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Paul%20D.%22%2C%22lastName%22%3A%22Drew%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Jennifer%20W.%22%2C%22lastName%22%3A%22Johnson%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22James%20C.%22%2C%22lastName%22%3A%22Douglas%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Kevin%20D.%22%2C%22lastName%22%3A%22Phelan%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Cynthia%20J.%20M.%22%2C%22lastName%22%3A%22Kane%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%2203%5C%2F2015%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1111%5C%2Facer.12639%22%2C%22ISSN%22%3A%2201456008%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fdoi.wiley.com%5C%2F10.1111%5C%2Facer.12639%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222015-08-17T17%3A18%3A46Z%22%7D%7D%2C%7B%22key%22%3A%22VUMRWEAW%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Eriksson%20et%20al.%22%2C%22parsedDate%22%3A%222015%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3EEriksson%2C%20A.%2C%20Williams%2C%20M.%20J.%2C%20Voisin%2C%20S.%2C%20Hansson%2C%20I.%2C%20Krishnan%2C%20A.%2C%20Philippot%2C%20G.%2C%20Yamskova%2C%20O.%2C%20Herisson%2C%20F.%20M.%2C%20Dnyansagar%2C%20R.%2C%20Moschonis%2C%20G.%2C%20Manios%2C%20Y.%2C%20Chrousos%2C%20G.%20P.%2C%20Olszewski%2C%20P.%20K.%2C%20Frediksson%2C%20R.%2C%20%26amp%3B%20Schi%26%23xF6%3Bth%2C%20H.%20B.%20%282015%29.%20Implication%20of%20coronin%207%20in%20body%20weight%20regulation%20in%20humans%2C%20mice%20and%20flies.%20%3Ci%3EBMC%20Neuroscience%3C%5C%2Fi%3E%2C%20%3Ci%3E16%3C%5C%2Fi%3E%281%29%2C%2013.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1186%5C%2Fs12868-015-0151-9%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1186%5C%2Fs12868-015-0151-9%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Implication%20of%20coronin%207%20in%20body%20weight%20regulation%20in%20humans%2C%20mice%20and%20flies%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Anders%22%2C%22lastName%22%3A%22Eriksson%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Michael%20J%22%2C%22lastName%22%3A%22Williams%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Sarah%22%2C%22lastName%22%3A%22Voisin%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Ida%22%2C%22lastName%22%3A%22Hansson%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Arunkumar%22%2C%22lastName%22%3A%22Krishnan%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Gaetan%22%2C%22lastName%22%3A%22Philippot%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Olga%22%2C%22lastName%22%3A%22Yamskova%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Florence%20M%22%2C%22lastName%22%3A%22Herisson%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Rohit%22%2C%22lastName%22%3A%22Dnyansagar%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22George%22%2C%22lastName%22%3A%22Moschonis%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Yannis%22%2C%22lastName%22%3A%22Manios%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22George%20P%22%2C%22lastName%22%3A%22Chrousos%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Pawel%20K%22%2C%22lastName%22%3A%22Olszewski%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Robert%22%2C%22lastName%22%3A%22Frediksson%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Helgi%20B%22%2C%22lastName%22%3A%22Schi%5Cu00f6th%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222015%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1186%5C%2Fs12868-015-0151-9%22%2C%22ISSN%22%3A%221471-2202%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fwww.biomedcentral.com%5C%2F1471-2202%5C%2F16%5C%2F13%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222015-12-31T20%3A09%3A52Z%22%7D%7D%2C%7B%22key%22%3A%22ZSDQPZXI%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Hu%20et%20al.%22%2C%22parsedDate%22%3A%222015%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3EHu%2C%20V.%20W.%2C%20Sarachana%2C%20T.%2C%20Sherrard%2C%20R.%20M.%2C%20%26amp%3B%20Kocher%2C%20K.%20M.%20%282015%29.%20Investigation%20of%20sex%20differences%20in%20the%20expression%20of%20RORA%20and%20its%20transcriptional%20targets%20in%20the%20brain%20as%20a%20potential%20contributor%20to%20the%20sex%20bias%20in%20autism.%20%3Ci%3EMolecular%20Autism%3C%5C%2Fi%3E%2C%20%3Ci%3E6%3C%5C%2Fi%3E%281%29%2C%207.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1186%5C%2F2040-2392-6-7%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1186%5C%2F2040-2392-6-7%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Investigation%20of%20sex%20differences%20in%20the%20expression%20of%20RORA%20and%20its%20transcriptional%20targets%20in%20the%20brain%20as%20a%20potential%20contributor%20to%20the%20sex%20bias%20in%20autism%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Valerie%20W%22%2C%22lastName%22%3A%22Hu%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Tewarit%22%2C%22lastName%22%3A%22Sarachana%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Rachel%20M%22%2C%22lastName%22%3A%22Sherrard%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Kristen%20M%22%2C%22lastName%22%3A%22Kocher%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222015%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1186%5C%2F2040-2392-6-7%22%2C%22ISSN%22%3A%222040-2392%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fwww.molecularautism.com%5C%2Fcontent%5C%2F6%5C%2F1%5C%2F7%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222015-12-31T18%3A07%3A32Z%22%7D%7D%2C%7B%22key%22%3A%2248PUC8WE%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Yoshida%20et%20al.%22%2C%22parsedDate%22%3A%222014-12-01%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3EYoshida%2C%20Y.%2C%20Ozawa%2C%20T.%2C%20Yao%2C%20T.-W.%2C%20Shen%2C%20W.%2C%20Brown%2C%20D.%2C%20Parsa%2C%20A.%20T.%2C%20Raizer%2C%20J.%20J.%2C%20Cheng%2C%20S.-Y.%2C%20Stegh%2C%20A.%20H.%2C%20Mazar%2C%20A.%20P.%2C%20Giles%2C%20F.%20J.%2C%20Sarkaria%2C%20J.%20N.%2C%20Butowski%2C%20N.%2C%20Nicolaides%2C%20T.%2C%20%26amp%3B%20James%2C%20C.%20D.%20%282014%29.%20NT113%2C%20a%20Pan-ERBB%20Inhibitor%20with%20High%20Brain%20Penetrance%2C%20Inhibits%20the%20Growth%20of%20Glioblastoma%20Xenografts%20with%20EGFR%20Amplification.%20%3Ci%3EMolecular%20Cancer%20Therapeutics%3C%5C%2Fi%3E%2C%20%3Ci%3E13%3C%5C%2Fi%3E%2812%29%2C%202919%26%23x2013%3B2929.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1158%5C%2F1535-7163.MCT-14-0306%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1158%5C%2F1535-7163.MCT-14-0306%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22NT113%2C%20a%20Pan-ERBB%20Inhibitor%20with%20High%20Brain%20Penetrance%2C%20Inhibits%20the%20Growth%20of%20Glioblastoma%20Xenografts%20with%20EGFR%20Amplification%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Y.%22%2C%22lastName%22%3A%22Yoshida%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22T.%22%2C%22lastName%22%3A%22Ozawa%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22T.-W.%22%2C%22lastName%22%3A%22Yao%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22W.%22%2C%22lastName%22%3A%22Shen%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22D.%22%2C%22lastName%22%3A%22Brown%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22A.%20T.%22%2C%22lastName%22%3A%22Parsa%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22J.%20J.%22%2C%22lastName%22%3A%22Raizer%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22S.-Y.%22%2C%22lastName%22%3A%22Cheng%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22A.%20H.%22%2C%22lastName%22%3A%22Stegh%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22A.%20P.%22%2C%22lastName%22%3A%22Mazar%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22F.%20J.%22%2C%22lastName%22%3A%22Giles%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22J.%20N.%22%2C%22lastName%22%3A%22Sarkaria%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22N.%22%2C%22lastName%22%3A%22Butowski%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22T.%22%2C%22lastName%22%3A%22Nicolaides%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22C.%20D.%22%2C%22lastName%22%3A%22James%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222014-12-01%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1158%5C%2F1535-7163.MCT-14-0306%22%2C%22ISSN%22%3A%221535-7163%2C%201538-8514%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fmct.aacrjournals.org%5C%2Fcgi%5C%2Fdoi%5C%2F10.1158%5C%2F1535-7163.MCT-14-0306%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222016-01-13T18%3A42%3A34Z%22%7D%7D%2C%7B%22key%22%3A%22WJSWUTEG%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Zhou%20et%20al.%22%2C%22parsedDate%22%3A%222014-11-01%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3EZhou%2C%20C.%2C%20Chen%2C%20J.%2C%20Zhang%2C%20X.%2C%20Costa%2C%20L.%20G.%2C%20%26amp%3B%20Guizzetti%2C%20M.%20%282014%29.%20Prenatal%20Ethanol%20Exposure%20Up-Regulates%20the%20Cholesterol%20Transporters%20ATP-Binding%20Cassette%20A1%20and%20G1%20and%20Reduces%20Cholesterol%20Levels%20in%20the%20Developing%20Rat%20Brain.%20%3Ci%3EAlcohol%20and%20Alcoholism%3C%5C%2Fi%3E%2C%20%3Ci%3E49%3C%5C%2Fi%3E%286%29%2C%20626%26%23x2013%3B634.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1093%5C%2Falcalc%5C%2Fagu049%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1093%5C%2Falcalc%5C%2Fagu049%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Prenatal%20Ethanol%20Exposure%20Up-Regulates%20the%20Cholesterol%20Transporters%20ATP-Binding%20Cassette%20A1%20and%20G1%20and%20Reduces%20Cholesterol%20Levels%20in%20the%20Developing%20Rat%20Brain%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22C.%22%2C%22lastName%22%3A%22Zhou%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22J.%22%2C%22lastName%22%3A%22Chen%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22X.%22%2C%22lastName%22%3A%22Zhang%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22L.%20G.%22%2C%22lastName%22%3A%22Costa%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22M.%22%2C%22lastName%22%3A%22Guizzetti%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222014-11-01%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1093%5C%2Falcalc%5C%2Fagu049%22%2C%22ISSN%22%3A%220735-0414%2C%201464-3502%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fwww.alcalc.oxfordjournals.org%5C%2Fcgi%5C%2Fdoi%5C%2F10.1093%5C%2Falcalc%5C%2Fagu049%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222015-08-03T16%3A02%3A56Z%22%7D%7D%2C%7B%22key%22%3A%2253TPMHQG%22%2C%22library%22%3A%7B%22id%22%3A2474232%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Terryn%20et%20al.%22%2C%22parsedDate%22%3A%222014-10-27%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%202%3B%20padding-left%3A%201em%3B%20text-indent%3A-1em%3B%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%3ETerryn%2C%20S.%2C%20Francart%2C%20A.%2C%20Lamoral%2C%20S.%2C%20Hultberg%2C%20A.%2C%20Rommelaere%2C%20H.%2C%20Wittelsberger%2C%20A.%2C%20Callewaert%2C%20F.%2C%20Stohr%2C%20T.%2C%20Meerschaert%2C%20K.%2C%20Ottevaere%2C%20I.%2C%20Stortelers%2C%20C.%2C%20Vanlandschoot%2C%20P.%2C%20Kalai%2C%20M.%2C%20%26amp%3B%20Van%20Gucht%2C%20S.%20%282014%29.%20Protective%20Effect%20of%20Different%20Anti-Rabies%20Virus%20VHH%20Constructs%20against%20Rabies%20Disease%20in%20Mice.%20%3Ci%3EPLoS%20ONE%3C%5C%2Fi%3E%2C%20%3Ci%3E9%3C%5C%2Fi%3E%2810%29%2C%20e109367.%20%3Ca%20class%3D%27zp-DOIURL%27%20href%3D%27https%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1371%5C%2Fjournal.pone.0109367%27%3Ehttps%3A%5C%2F%5C%2Fdoi.org%5C%2F10.1371%5C%2Fjournal.pone.0109367%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Protective%20Effect%20of%20Different%20Anti-Rabies%20Virus%20VHH%20Constructs%20against%20Rabies%20Disease%20in%20Mice%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Sanne%22%2C%22lastName%22%3A%22Terryn%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Aur%5Cu00e9lie%22%2C%22lastName%22%3A%22Francart%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Sophie%22%2C%22lastName%22%3A%22Lamoral%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Anna%22%2C%22lastName%22%3A%22Hultberg%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Heidi%22%2C%22lastName%22%3A%22Rommelaere%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Angela%22%2C%22lastName%22%3A%22Wittelsberger%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Filip%22%2C%22lastName%22%3A%22Callewaert%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Thomas%22%2C%22lastName%22%3A%22Stohr%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Kris%22%2C%22lastName%22%3A%22Meerschaert%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Ingrid%22%2C%22lastName%22%3A%22Ottevaere%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Catelijne%22%2C%22lastName%22%3A%22Stortelers%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Peter%22%2C%22lastName%22%3A%22Vanlandschoot%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Michael%22%2C%22lastName%22%3A%22Kalai%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Steven%22%2C%22lastName%22%3A%22Van%20Gucht%22%7D%2C%7B%22creatorType%22%3A%22editor%22%2C%22firstName%22%3A%22Matthias%20Johannes%22%2C%22lastName%22%3A%22Schnell%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222014-10-27%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1371%5C%2Fjournal.pone.0109367%22%2C%22ISSN%22%3A%221932-6203%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fdx.plos.org%5C%2F10.1371%5C%2Fjournal.pone.0109367%22%2C%22collections%22%3A%5B%22M2MNG549%22%5D%2C%22dateModified%22%3A%222015-09-01T19%3A30%3A46Z%22%7D%7D%5D%7D
Mahinrad, S., Bulk, M., van der Velpen, I., Mahfouz, A., van Roon-Mom, W., Fedarko, N., Yasar, S., Sabayan, B., van Heemst, D., & van der Weerd, L. (2018). Natriuretic Peptides in Post-mortem Brain Tissue and Cerebrospinal Fluid of Non-demented Humans and Alzheimer’s Disease Patients. Frontiers in Neuroscience, 12, 864. https://doi.org/10.3389/fnins.2018.00864
Kim, J. M., Park, S. K., Guo, T. J., Kang, J. Y., Ha, J. S., Lee, D. S., Lee, U., & Heo, H. J. (2016). Anti-amnesic effect of Dendropanax morbifera via JNK signaling pathway on cognitive dysfunction in high-fat diet-induced diabetic mice. Behavioural Brain Research, 312, 39–54. https://doi.org/10.1016/j.bbr.2016.06.013
Murray, H. C., Low, V. F., Swanson, M. E. V., Dieriks, B. V., Turner, C., Faull, R. L. M., & Curtis, M. A. (2016). Distribution of PSA-NCAM in normal, Alzheimer’s and Parkinson’s disease human brain. Neuroscience, 330, 359–375. https://doi.org/10.1016/j.neuroscience.2016.06.003
David, C. N., Frias, E. S., Szu, J. I., Vieira, P. A., Hubbard, J. A., Lovelace, J., Michael, M., Worth, D., McGovern, K. E., Ethell, I. M., Stanley, B. G., Korzus, E., Fiacco, T. A., Binder, D. K., & Wilson, E. H. (2016). GLT-1-Dependent Disruption of CNS Glutamate Homeostasis and Neuronal Function by the Protozoan Parasite Toxoplasma gondii. PLOS Pathog, 12(6), e1005643. https://doi.org/10.1371/journal.ppat.1005643
Perland, E., Lekholm, E., Eriksson, M. M., Bagchi, S., Arapi, V., & Fredriksson, R. (2016). The Putative SLC Transporters Mfsd5 and Mfsd11 Are Abundantly Expressed in the Mouse Brain and Have a Potential Role in Energy Homeostasis. PLOS ONE, 11(6), e0156912. https://doi.org/10.1371/journal.pone.0156912
Kumar, M., Belcaid, M., & Nerurkar, V. R. (2016). Identification of host genes leading to West Nile virus encephalitis in mice brain using RNA-seq analysis. Scientific Reports, 6. https://doi.org/10.1038/srep26350
Vadnie, C. A., Ayers-Ringler, J., Oliveros, A., Abulseoud, O. A., Choi, S., Hitschfeld, M. J., & Choi, D.-S. (2016). Antipsychotic-like effects of a neurotensin receptor type 1 agonist. Behavioural Brain Research, 305, 8–17. https://doi.org/10.1016/j.bbr.2016.02.019
Hoover, C. E., Davenport, K. A., Henderson, D. M., Pulscher, L. A., Mathiason, C. K., Zabel, M. D., & Hoover, E. A. (2016). Detection and Quantification of CWD Prions in Fixed Paraffin Embedded Tissues by Real-Time Quaking-Induced Conversion. Scientific Reports, 6. https://doi.org/10.1038/srep25098
Lui, H., Zhang, J., Makinson, S. R., Cahill, M. K., Kelley, K. W., Huang, H.-Y., Shang, Y., Oldham, M. C., Martens, L. H., Gao, F., Coppola, G., Sloan, S. A., Hsieh, C. L., Kim, C. C., Bigio, E. H., Weintraub, S., Mesulam, M.-M., Rademakers, R., Mackenzie, I. R., … Huang, E. J. (2016). Progranulin Deficiency Promotes Circuit-Specific Synaptic Pruning by Microglia via Complement Activation. Cell, 165(4), 921–935. https://doi.org/10.1016/j.cell.2016.04.001
Zeng, X., Wang, H., Xing, X., Wang, Q., & Li, W. (2016). Dexmedetomidine Protects against Transient Global Cerebral Ischemia/Reperfusion Induced Oxidative Stress and Inflammation in Diabetic Rats. PLOS ONE, 11(3), e0151620. https://doi.org/10.1371/journal.pone.0151620
Ayers-Ringler, J. R., Oliveros, A., Qiu, Y., Lindberg, D. M., Hinton, D. J., Moore, R. M., Dasari, S., & Choi, D.-S. (2016). Label-Free Proteomic Analysis of Protein Changes in the Striatum during Chronic Ethanol Use and Early Withdrawal. Frontiers in Behavioral Neuroscience, 10. https://doi.org/10.3389/fnbeh.2016.00046
Bosch, M., Fajardo, A., Alcalá-Vida, R., Fernández-Vidal, A., Tebar, F., Enrich, C., Cardellach, F., Pérez-Navarro, E., & Pol, A. (2016). Hepatic Primary and Secondary Cholesterol Deposition and Damage in Niemann-Pick Disease. The American Journal of Pathology, 186(3), 517–523. https://doi.org/10.1016/j.ajpath.2015.12.002
Bakmiwewa, S. M., Weiser, S., Grey, M., Heng, B., Guillemin, G. J., Ball, H. J., & Hunt, N. H. (2016). Synergistic induction of CXCL10 by interferon-gamma and lymphotoxin-alpha in astrocytes: Possible role in cerebral malaria. Cytokine, 78, 79–86. https://doi.org/10.1016/j.cyto.2015.11.024
Viader, A., Ogasawara, D., Joslyn, C. M., Sanchez-Alavez, M., Mori, S., Nguyen, W., Conti, B., & Cravatt, B. F. (2016). A chemical proteomic atlas of brain serine hydrolases identifies cell type-specific pathways regulating neuroinflammation. ELife, 5, e12345. https://doi.org/10.7554/eLife.12345
Hallgren, S., & Viberg, H. (2016). Postnatal exposure to PFOS, but not PBDE 99, disturb dopaminergic gene transcription in the mouse CNS. Environmental Toxicology and Pharmacology, 41, 121–126. https://doi.org/10.1016/j.etap.2015.11.016
Luethy, L. N., Erickson, A. K., Jesudhasan, P. R., Ikizler, M., Dermody, T. S., & Pfeiffer, J. K. (2016). Comparison of three neurotropic viruses reveals differences in viral dissemination to the central nervous system. Virology, 487, 1–10. https://doi.org/10.1016/j.virol.2015.09.019
Kim, J., Shim, J., Lee, S., Cho, W.-H., Hong, E., Lee, J. H., Han, J.-S., Lee, H. J., & Lee, K. W. (2016). Rg3-enriched ginseng extract ameliorates scopolamine-induced learning deficits in mice. BMC Complementary and Alternative Medicine, 16, 66. https://doi.org/10.1186/s12906-016-1050-z
Gallart-Palau, X., Serra, A., & Sze, S. K. (2016). Enrichment of extracellular vesicles from tissues of the central nervous system by PROSPR. Molecular Neurodegeneration, 11, 41. https://doi.org/10.1186/s13024-016-0108-1
Gallart-Palau, X., Lee, B. S. T., Adav, S. S., Qian, J., Serra, A., Park, J. E., Lai, M. K. P., Chen, C. P., Kalaria, R. N., & Sze, S. K. (2016). Gender differences in white matter pathology and mitochondrial dysfunction in Alzheimer’s disease with cerebrovascular disease. Molecular Brain, 9, 27. https://doi.org/10.1186/s13041-016-0205-7
Tristán-Noguero, A., Díez, H., Jou, C., Pineda, M., Ormazábal, A., Sánchez, A., Artuch, R., & Garcia-Cazorla, À. (2015). Study of a fetal brain affected by a severe form of tyrosine hydroxylase deficiency, a rare cause of early parkinsonism. Metabolic Brain Disease. https://doi.org/10.1007/s11011-015-9780-z
Hajkova, K., Jurasek, B., Sykora, D., Palenicek, T., Miksatkova, P., & Kuchar, M. (2015). Salting-out-assisted liquid–liquid extraction as a suitable approach for determination of methoxetamine in large sets of tissue samples. Analytical and Bioanalytical Chemistry. https://doi.org/10.1007/s00216-015-9221-1
Wang, Y., Billon, C., Walker, J. K., & Burris, T. P. (2015). Therapeutic Effect of a Synthetic RORα/γ Agonist in an Animal Model of Autism. ACS Chemical Neuroscience. https://doi.org/10.1021/acschemneuro.5b00159
Semple, B. D., Noble-Haeusslein, L. J., Gooyit, M., Tercovich, K. G., Peng, Z., Nguyen, T. T., Schroeder, V. A., Suckow, M. A., Chang, M., Raber, J., & Trivedi, A. (2015). Early Gelatinase Activity Is Not a Determinant of Long-Term Recovery after Traumatic Brain Injury in the Immature Mouse. PLOS ONE, 10(11), e0143386. https://doi.org/10.1371/journal.pone.0143386
Falendysz, E. A., Lopera, J. G., Lorenzsonn, F., Salzer, J. S., Hutson, C. L., Doty, J., Gallardo-Romero, N., Carroll, D. S., Osorio, J. E., & Rocke, T. E. (2015). Further Assessment of Monkeypox Virus Infection in Gambian Pouched Rats (Cricetomys gambianus) Using In Vivo Bioluminescent Imaging. PLOS Neglected Tropical Diseases, 9(10), e0004130. https://doi.org/10.1371/journal.pntd.0004130
Lee, M., Chen, Z., Tomlinson, B. N., Gooyit, M., Hesek, D., Juárez, M. R., Nizam, R., Boggess, B., Lastochkin, E., Schroeder, V. A., Wolter, W. R., Suckow, M. A., Cui, J., Mobashery, S., Gu, Z., & Chang, M. (2015). Water-Soluble MMP-9 Inhibitor Reduces Lesion Volume after Severe Traumatic Brain Injury. ACS Chemical Neuroscience, 6(10), 1658–1664. https://doi.org/10.1021/acschemneuro.5b00140
Yau, B., Mitchell, A. J., Too, L. K., Ball, H. J., & Hunt, N. H. (2015). Interferon-γ-Induced Nitric Oxide Synthase-2 Contributes to Blood/Brain Barrier Dysfunction and Acute Mortality in Experimental Streptococcus pneumoniae Meningitis. Journal of Interferon & Cytokine Research. https://doi.org/10.1089/jir.2015.0078
Crowell, J., Hughson, A., Caughey, B., & Bessen, R. A. (2015). Host determinants of prion strain diversity independent of prion protein genotype. Journal of Virology, JVI.01586-15. https://doi.org/10.1128/JVI.01586-15
Xu, X.-F., Li, T., Wang, D.-D., Chen, B., Wang, Y., & Chen, Z.-Y. (2015). Integrin-linked Kinase is Essential for Environmental Enrichment Enhanced Hippocampal Neurogenesis and Memory. Scientific Reports, 5, 11456. https://doi.org/10.1038/srep11456
Grasso, C. S., Tang, Y., Truffaux, N., Berlow, N. E., Liu, L., Debily, M.-A., Quist, M. J., Davis, L. E., Huang, E. C., Woo, P. J., Ponnuswami, A., Chen, S., Johung, T. B., Sun, W., Kogiso, M., Du, Y., Qi, L., Huang, Y., Hütt-Cabezas, M., … Monje, M. (2015). Functionally defined therapeutic targets in diffuse intrinsic pontine glioma. Nature Medicine, 21(6), 555–559. https://doi.org/10.1038/nm.3855
Ciesielska, A., Sharma, N., Beyer, J., Forsayeth, J., & Bankiewicz, K. (2015). Carbidopa-Based Modulation of the Functional Effect of the AAV2-hAADC Gene Therapy in 6-OHDA Lesioned Rats. PLOS ONE, 10(4), e0122708. https://doi.org/10.1371/journal.pone.0122708
Crowell, J., Wiley, J. A., & Bessen, R. A. (2015). Lesion of the Olfactory Epithelium Accelerates Prion Neuroinvasion and Disease Onset when Prion Replication Is Restricted to Neurons. PLOS ONE, 10(3), e0119863. https://doi.org/10.1371/journal.pone.0119863
Wang, H., Yang, Y., Li, Y., Bai, B., Wang, X., Tan, H., Liu, T., Beach, T. G., Peng, J., & Wu, Z. (2015). Systematic Optimization of Long Gradient Chromatography Mass Spectrometry for Deep Analysis of Brain Proteome. Journal of Proteome Research, 14(2), 829–838. https://doi.org/10.1021/pr500882h
Burrell-Saward, H. (2015). Development of an imaging model of a CNS infection with African trypanosomes. [London School of Hygeine and Tropical Medicine]. http://researchonline.lshtm.ac.uk/2222110/1/2015_ITD_PhD_Burrell-Saward_H.pdf
Evers, M. M., Schut, M. H., Pepers, B. A., Atalar, M., van Belzen, M. J., Faull, R. L., Roos, R. A., & van Roon-Mom, W. M. (2015). Making (anti-) sense out of huntingtin levels in Huntington disease. Molecular Neurodegeneration, 10(1). https://doi.org/10.1186/s13024-015-0018-7
Doldur-Balli, F., Ozel, M. N., Gulsuner, S., Tekinay, A. B., Ozcelik, T., Konu, O., & Adams, M. M. (2015). Characterization of a novel zebrafish (Danio rerio) gene, wdr81, associated with cerebellar ataxia, mental retardation and dysequilibrium syndrome (CAMRQ). BMC Neuroscience, 16(1). https://doi.org/10.1186/s12868-015-0229-4
Kumar, M., Roe, K., O’Connell, M., & Nerurkar, V. R. (2015). Induction of virus-specific effector immune cell response limits virus replication and severe disease in mice infected with non-lethal West Nile virus Eg101 strain. Journal of Neuroinflammation, 12(1). https://doi.org/10.1186/s12974-015-0400-y
Khademi, S., Frye, M. A., Jeckel, K. M., Schroeder, T., Monnet, E., Irwin, D. C., Cole, P. A., Bell, C., Miller, B. F., & Hamilton, K. L. (2015). Hypoxia mediated pulmonary edema: potential influence of oxidative stress, sympathetic activation and cerebral blood flow. BMC Physiology, 15(1). https://doi.org/10.1186/s12899-015-0018-4
Yuan, Z.-X., & Rapoport, S. I. (2015). Transient postnatal fluoxetine decreases brain concentrations of 20-HETE and 15-epi-LXA4, arachidonic acid metabolites in adult mice. Prostaglandins, Leukotrienes and Essential Fatty Acids (PLEFA), 101, 9–14. https://doi.org/10.1016/j.plefa.2015.07.002
Wong, R. Y., & Godwin, J. (2015). Neurotranscriptome profiles of multiple zebrafish strains. Genomics Data, 5, 206–209. https://doi.org/10.1016/j.gdata.2015.06.004
Hallgren, S., Fredriksson, A., & Viberg, H. (2015). More signs of neurotoxicity of surfactants and flame retardants – Neonatal PFOS and PBDE 99 cause transcriptional alterations in cholinergic genes in the mouse CNS. Environmental Toxicology and Pharmacology, 40(2), 409–416. https://doi.org/10.1016/j.etap.2015.06.014
Zhou, J., Coles, L. D., Kartha, R. V., Nash, N., Mishra, U., Lund, T. C., & Cloyd, J. C. (2015). Intravenous Administration of Stable-Labeled N-Acetylcysteine Demonstrates an Indirect Mechanism for Boosting Glutathione and Improving Redox Status. Journal of Pharmaceutical Sciences, 104(8), 2619–2626. https://doi.org/10.1002/jps.24482
Razafsky, D., & Hodzic, D. (2015). A variant of Nesprin1 giant devoid of KASH domain underlies the molecular etiology of autosomal recessive cerebellar ataxia type I. Neurobiology of Disease, 78, 57–67. https://doi.org/10.1016/j.nbd.2015.03.027
Aryal, M., Vykhodtseva, N., Zhang, Y.-Z., & McDannold, N. (2015). Multiple sessions of liposomal doxorubicin delivery via focused ultrasound mediated blood–brain barrier disruption: A safety study. Journal of Controlled Release, 204, 60–69. https://doi.org/10.1016/j.jconrel.2015.02.033
Hägglund, M. G. A., Hellsten, S. V., Bagchi, S., Philippot, G., Löfqvist, E., Nilsson, V. C. O., Almkvist, I., Karlsson, E., Sreedharan, S., Tafreshiha, A., & Fredriksson, R. (2015). Transport of l-Glutamine, l-Alanine, l-Arginine and l-Histidine by the Neuron-Specific Slc38a8 (SNAT8) in CNS. Journal of Molecular Biology, 427(6), 1495–1512. https://doi.org/10.1016/j.jmb.2014.10.016
Drew, P. D., Johnson, J. W., Douglas, J. C., Phelan, K. D., & Kane, C. J. M. (2015). Pioglitazone Blocks Ethanol Induction of Microglial Activation and Immune Responses in the Hippocampus, Cerebellum, and Cerebral Cortex in a Mouse Model of Fetal Alcohol Spectrum Disorders. Alcoholism: Clinical and Experimental Research, 39(3), 445–454. https://doi.org/10.1111/acer.12639
Eriksson, A., Williams, M. J., Voisin, S., Hansson, I., Krishnan, A., Philippot, G., Yamskova, O., Herisson, F. M., Dnyansagar, R., Moschonis, G., Manios, Y., Chrousos, G. P., Olszewski, P. K., Frediksson, R., & Schiöth, H. B. (2015). Implication of coronin 7 in body weight regulation in humans, mice and flies. BMC Neuroscience, 16(1), 13. https://doi.org/10.1186/s12868-015-0151-9
Hu, V. W., Sarachana, T., Sherrard, R. M., & Kocher, K. M. (2015). Investigation of sex differences in the expression of RORA and its transcriptional targets in the brain as a potential contributor to the sex bias in autism. Molecular Autism, 6(1), 7. https://doi.org/10.1186/2040-2392-6-7
Yoshida, Y., Ozawa, T., Yao, T.-W., Shen, W., Brown, D., Parsa, A. T., Raizer, J. J., Cheng, S.-Y., Stegh, A. H., Mazar, A. P., Giles, F. J., Sarkaria, J. N., Butowski, N., Nicolaides, T., & James, C. D. (2014). NT113, a Pan-ERBB Inhibitor with High Brain Penetrance, Inhibits the Growth of Glioblastoma Xenografts with EGFR Amplification. Molecular Cancer Therapeutics, 13(12), 2919–2929. https://doi.org/10.1158/1535-7163.MCT-14-0306
Zhou, C., Chen, J., Zhang, X., Costa, L. G., & Guizzetti, M. (2014). Prenatal Ethanol Exposure Up-Regulates the Cholesterol Transporters ATP-Binding Cassette A1 and G1 and Reduces Cholesterol Levels in the Developing Rat Brain. Alcohol and Alcoholism, 49(6), 626–634. https://doi.org/10.1093/alcalc/agu049
Terryn, S., Francart, A., Lamoral, S., Hultberg, A., Rommelaere, H., Wittelsberger, A., Callewaert, F., Stohr, T., Meerschaert, K., Ottevaere, I., Stortelers, C., Vanlandschoot, P., Kalai, M., & Van Gucht, S. (2014). Protective Effect of Different Anti-Rabies Virus VHH Constructs against Rabies Disease in Mice. PLoS ONE, 9(10), e109367. https://doi.org/10.1371/journal.pone.0109367